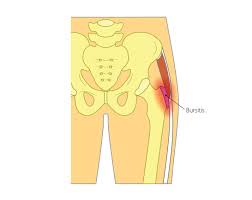
 Characterized by painful inflammation of the bursa located just superficial to the greater trochanter of the femur.
Characterized by painful inflammation of the bursa located just superficial to the greater trochanter of the femur.
The trochanteric bursa is at the top, outer side of the femur, between the insertion of the gluteus medius and gluteus minimus muscles into the greater trochanter of the femur and the femoral shaft.
It has the function, in common with other bursae, of working as a shock absorber and as a lubricant for the movement of the muscles adjacent to it.
Patients typically complain of lateral hip pain.
Occasionally, this bursa can become inflamed and clinically painful and tender.
This condition can be a manifestation of an injury, avtwisting motion or from overuse, but sometimes arises for no obviously definable cause.
The hip joint itself is not involved.
The pain may radiate down the lateral aspect of the thigh.
The symptoms are pain in the hip region on walking, and tenderness over the upper part of the femur, which may result in the inability to lie in comfort on the affected side.
The term greater trochanteric pain syndrome (GTPS) is now being commonly substituted, because the inflammatory etiology of the pain is being refuted.
Inflammation of the affected bursa between the femoral trochanteric process and the gluteus medius/iliotibial tract may be caused by acute or repetitive trauma.
Acute trauma that can cause trochanteric bursitis may be caused by falls, sports injuries, and other types of impact.
Repetitive trauma includes bursal irritation resulting from friction by the iliotibial band (an extension of the tensor fascia lata muscle) occurs in runners.
More often the lateral hip pain is caused by disease of the gluteal tendons that secondarily inflames the bursa.
This is most common in middle-aged women and is associated with a chronic and debilitating pain which does not respond to conservative treatment.
Other causes of trochanteric bursitis include uneven leg length, iliotibial band syndrome, and weakness of the hip abductor muscles.
Relatively common in physically active patients.
May occur in sedentary individuals.
Unilateral and bilateral greater trochanteric pain syndrome has a prevalence of 15.0% and 8.5% in women, and of 6.6% and 1.9% men, respectively.
Annual incidence in primary care reported as being 1.8 patients per 1000.
Associated with chronic pain, limping and difficulty with sleeping.
Female:male 80%:20%.
Can occur at any age.
Lateral hip pain is the classic presentation.
Pain increased by lying down on the affected bursa and is exacerbated by walking, running and weight bearing with internal and external hip rotation.
The patient may be report weakness of the leg due to pain.
Classically point tenderness is present over the greater trochanter, reproducing symptoms.
Lateral hip pain can often be elicited by passive external rotation of the hip.
Lateral hip pain can be reproduced with flexion of the hip.
Differential diagnosis: Osteoarthritis, fracture of the femur, avascular necrosis of the femoral head, lumbosacral radiculopathy, gluteus medius bursitis,glucose medius partial tear, iliopsoas bursitis, and iliotibial band tenditis.
Diagnosis is clinically based and radiographic imaging may be performed to rule out other entities.
Greater trochanteric pain syndrome can remain incorrectly diagnosed for years, because it shares the same pattern of pain with many other musculoskeletal conditions.
Palpating the hip and leg may reveal the location of the pain, and range-of-motion tests can help to identify its source.
X-rays, ultrasound and magnetic resonance imaging may reveal tears or swelling.
But often these imaging tests do not reveal any obvious abnormality in patients with documented GTPS.
Injection of local anesthetic into the trochanteric bursa may be helpful in confirming the diagnosis.
Treatment:
Conservative treatments have a 90% success rate and can include any or a combination of the following: pain relief medication, NSAIDs, physiotherapy, shockwave therapy (SWT) and corticosteroid injection.
Surgery is usually for cases that are non-respondent to conservative treatments and is often a combination of bursectomy, iliotibial band (ITB) release, trochanteric reduction osteotomy or gluteal tendon repair.
The primary treatment is rest, by avoiding actions which result in aggravation of the pain.
Icing the joint may help.
A non-steroidal anti-inflammatory drug may relieve pain and reduce the inflammation.
Definitive treatment is steroid injection into the inflamed area.
Physical therapy to strengthen the hip muscles and stretch the iliotibial band can relieve tension in the hip and reduce friction.
Corticosteroid and lidocaine injections into the bursa is an effective therapy with a prolonged benefit.
Physical therapy, NSAIDs are often employed in management.
