
 Most common vasculitis involving older people.
Most common vasculitis involving older people.
Also known as giant cell arteritis.
A large vessel vasculopathy preferentially involving the aorta and the extracranial branches of the carotid (Salvarani C et al).
A chronic autoimmune inflammatory disorder affecting the major branches of the carotid artery.
Involves an antigen- immune response in blood vessel walls.
Ischemia results from downstream occlusion of vessels due to hyperplasia of cell wall components.
Effects the major branches of the carotid artery.
Thinning of media of the aorta is the only vessel of concern, and may lead to aneurysm.
In smaller blood vessels media is clinically insignificant.
Occlusion of the lumen of some vessels is his source of damage to downstream structures such as the optic nerve.
T-cell and T cell receptors are in adjacent and nonadjacent lesions.
T-cells and macrophages produce cytokines and growth factors with a cascade of inflammation ensuing leading to break down in the internal elastic lamina.
Breakdown in the presence of platelets-drived growth factors from multigiant cells proliferate the intimal layers leading to the occlusion of the lumen and downstream ischemia.
Typically affects patients over 50 years of age.
Peak incidence between 60 and 75.
Does not occur before age 50.
Incidence increases with advancing age.
Females twice the risk.
Disease almost always in Caucaians.
Clinical presentation is nonspecific with anorexia, weight loss, fatigue, and fever.
Neurologic manifestations include ischemic stroke.
Pulmonary and coronary artery may be affected and myocardial infarct is a possibility.
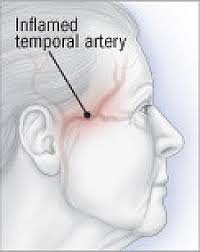
Headache most common symptom.
Temple pain is most common headache.
High fever persists in 10% of patients.
Jaw claudication, scalp tenderness, general malaise, weight loss and joint pain common symptoms.
Occasionally fever is accompanied by a rigors and sweats imitating sepsis.
Vision loss is less frequent presentation.
Elevated erythrocyte sedimentation rate is non-specific finding.
- Corticosteroids for up to seven years.
Adding aspirin to steroid therapy reduces the chance of recurrence.
There is approximately four week race period during which temporal artery biopsy results are unaltered due to steroid therapy.
Biopsy occurs under local anesthesia, at the frontal branch of the temporal artery as it is palpable.
Facial nerve damage may occur during the biopsy because the nerve has proximity to the front of branch of the temporal artery.
