 Right heart catheterization (RHC), or pulmonary artery catheterization, provides information about hemodynamics of the circulation.
Right heart catheterization (RHC), or pulmonary artery catheterization, provides information about hemodynamics of the circulation.
It assesses pressure waves generated by the different cardiac chambers.
It is used to differentiate forms of shock, cardiac vs non-cardiac, measures cardiac output, monitors the effect of inotropic and vasopressive medication, differentiated origin of pulmonary hypertension (primary vs secondary), assesses valve abnormalities, cardiac shunts and tamponade.
Simultaneous measurement of left and right sided pressures can be used to precisely determine whether constrictive pericarditis is present.
Its use has fallen because left heart catheterization alone is adequate for most patients undergoing evaluation of coronary artery disease.
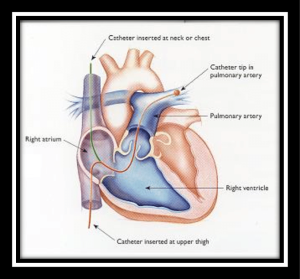
For right sided pressure monitoring a catheter is inserted into the pulmonary artery (Swan-Ganz catheter).
The catheter is a 5-7 french catheter which consists of 2-5 lumina with different purposes: a lumen for inflation of the balloon, a proximal and distal lumen for infusion of fluid or extraction of blood, a temperature thermistor and one for RV pacing.
Following local anesthesia, the femoral, jugular, brachial or subclavian vein is punctured, then a guidewire is introduced into the vein by Seldinger technique, and next a sheath is introduced.
Femoral access is associated with increased risk of local hemorrhage.
If the catheter is left indwelling, the jugular or subclavian vein is preferable, because it allows the patient to sit.
The jugular approach is preferred to the subclavian to lessen the risk of pneumothorax and is easiest performed ultrasound guided.
After placement of the sheath, the catheter is introduced into the vein and advanced into the inferior vena cava, superior vena cava, right atrium, right ventricle and pulmonary artery.
Normal Pressures and Vascular Resistances
Pressures Average (mm Hg) Range (mm Hg)
Right atrium
a wave 6 2-7
v wave 5 2-7
Mean 1-5
Right ventricle
Peak systolic 25 15-30
End-diastolic 4 1-7
Pulmonary artery
Peak systolic 25 15-30
End-diastolic 9 4-12
Mean 15 9-19
Pulmonary capillary
Wedge
Mean 9 4-12
Left atrium
a wave 10 4-16
v wave 12 6-21
Mean 8 2-12
Left ventricle
Peak systolic 130 90-140
End-diastolic 8 5-12
Central aorta
Peak systolic 130 90-140
End-diastolic 70 60-90
Mean 85 70-105
Vascular Resistance Mean (dyne-sec · cm -5) Range (dyne-sec · cm -5)
Right atrium
Systemic vascular resistance 1100 700-1600
Total pulmonary resistance 200 100-300
Pulmonary vascular resistance 70 20-130
Right atrium
a = atrial systole
x= atrial relaxation, decrease of pressure
c= closure of the tricuspid valve
v= ventricular systole, atrial diastole
y= passive filling of right ventricle
Normal RA pressure = 6 mmHg (3 mean)
Higher RA pressure in RV infarction, pulmonary hypertension, left to right shunts, tricuspid regurgitation, tamponade, pericarditis constrictiva, restrictive cardiomyopathy.
Abnormal right atrium pressure waves:
Elevated a wave: tricuspid stenosis, decreased ventricular compliance due to ventricular failure, pulmonic valve stenosis
Absent a wave: atrial fibrillation
Sawtooth a wave: atrial flutter
Elevated v wave: tricuspid regurgitation with prominent y descent, RV failure
Prominent x descent: tamponade
Kussmaul sign: constrictive pericarditis, RV ischemia?
Normal RV pressure = 25 / 4 mmHg
When there are no abnormalities in the right heart: CVP = RA pressure = RVEDP.
The pressure curve consists of a fast upstroke, a rounded top, directly after the QRS complex.
Higher RV pressure in pulmonary hypertension, pulmonic valve stenosis, significant ASD or VSD, pulmonary embolism.
Abnormal right ventricle pressure waves:
Systolic pressure reduced: hypovolemia, cardiogenic shock, tamponade
Elevated end diastolic pressure: cardiomyopathy, RV ischemia and infarction, RV failure, tamponade, pericarditis constrictiva
Decreased end diastolic pressure: tricuspid stenosis
Dip-and-plateau in constrictive pericarditis and restrictive myopathies
Pulmonary artery pressure
Normal PA pressure 25 / 9 mmHg (mean 15)
Abnormal pulmonary artery pressure waveforms
Elevated systolic pressure: idiopathic pulmonary hypertension, pulmonary disease, hypoxemia with pulmonary vasoconstriction, mitral stenosis or regurgitation, restrictive cardiomyopathies, significant cardiac left to right shunt, pulmonary embolism
Reduced pulce pressure: RV ischaemia or infarction, pulmonary embolism, tamponade
Pulmonary capillary wedge pressure (PCWP)
Normal PCWP pressure range = 4-12 mmHg (mean 9).
When there is no obstruction between left atrium and left ventricle: PCWP = LA pressure = LVEDP ( left ventricle end diastolic pressure).
Wedge pressure can be measured only in the absence of flow, with a vessel closed for flow by a balloon.
Normally PCWP equals LAP equals LVEDP.
The PCWP is higher than the LVEDP in:
Mitral stenosis
LA obstruction by myxoma
Mitral regurgitation
Pulmonary embolism or veno-occlusive disease
Respiratory failure (hypoxemia and pulmonary vasoconstriction)
The LVEDP is higher than the wedge in:
Diastolic dysfunction, positive end-expiratory airway pressure
Myocardial infarction
Tamponade
Aortic regurgitation (early closure mitral valve)
Abnormal PCWP pressure
Low mean pressure: hypovolemia
Elevated mean pressure: intravascular overload, LV failure caused by myocardial disease, systemic hypertension or valvular disease (MS, AoS, AoR), pericardial effusion with tamponade
Elevated a wave: mitral stenosis, diastolic dysfunction, LV volume overload
Cannon a wave due to atrial-ventricular asynchrony
Elevated v wave: mitral regurgitation, LV failure, VSD
Complications of right heart catheterization: rhythm disorders (atrial extrasystole, ventricular extrasystole, ventricular tachycardia, ventricular fibrillation), conduction disorders, damage to the pulmonic or tricuspid valve, thrombo-embolism of pulmonary infarction.
When performed at expert centers the procedure has low morbidity of about 1.1%, and mortality of 0.055%.
In 0.03-0.2% a pulmonary rupture is described as a right heart catheterization complication.
