 Percutaneous umbilical cord blood sampling (PUBS), also called cordocentesis, fetal blood sampling, or umbilical vein sampling.
Percutaneous umbilical cord blood sampling (PUBS), also called cordocentesis, fetal blood sampling, or umbilical vein sampling.
It is is a diagnostic genetic test that examines blood from the fetal umbilical cord to detect fetal abnormalities.
Fetal and maternal blood supply are typically connected in utero with one vein and two arteries to the fetus.
The umbilical vein is responsible for delivering oxygen rich blood to the fetus from the mother; the umbilical arteries are responsible for removing oxygen poor blood from the fetus.
PUBS provides a means for chromosome analysis and is useful when information cannot be obtained through amniocentesis, chorionic villus sampling, or ultrasound, or if the results of these tests were inconclusive.
PUBS carries a significant risk of complication and is typically reserved for pregnancies determined to be at high risk for genetic defect.
PUBS can also detect a number of abnormalities including pH levels, oxygen levels, chromosomal issues, and infections.
Fetoscopy is a procedure in which a device is inserted through the abdomen of the mother in order to visualize the fetus.
PUBS is not used often except when rapid diagnosis and decisions must be made in regards to the fetus and suspected abnormalities suspected.
PUBS has been predominantly replaced by Fluorescence in situ hybridization (FISH) which is a more detailed investigation of chromosomal abnormalities.
The procedure is performed close to an operating room in case an emergency cesarean section is necessary due to complications caused by the procedure.
Fetal viability typically occurs at about 24 to 25 weeks of gestation.
When the fetus is in between the ages of 24–34 weeks, a glucocorticoid is given to the patient about 24 hours before the procedure to stimulate lung maturity.
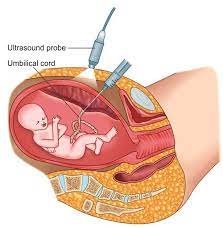
An ultrasound views the position of the fetus and may be used during the procedure to help guide the needle.
The mother’s blood is drawn for comparison against fetal blood.
To reduce the risk of intraamniotic infection, intravenous antibiotics are given about 30–60 minutes before the procedure.
This image shows anterior blood sampling from the umbilical cord.
A 20 or 22 gauge spinal needle is typically used in PUBS.
A typical sampling site would be where the segment of the umbilical cord is closest to the placenta.
Blood sampling is achieved more easily if the placenta is in the anterior position.
With the placenta in the posterior position, the fetus might block direct access to the umbilical cord.
The site of puncture is monitored after the procedure for bleeding, and the fetal heart rate is monitored post-procedure for one to two hours.
Fetal red blood cells are usually bigger than maternal RBCs: the mean corpuscular volume (MCV), is one of the methods used to determine whether or not the fetal blood has been contaminated.
Human chorionic gonadotropin (hCG) determination, can detect maternal blood because maternal blood has high levels of hCG.
The hemoglobin alkaline denaturation test (Apt test) can detect the presence of maternal blood.
Blood typing would also detect maternal blood : I antigen only occurs in adults.
The Kleihauer–Betke test can detect very small amounts of maternal blood before the third trimester of pregnancy by monitoring hemoglobin elution in acid because adult and fetal hemoglobin elute differently in acid.
A white blood cell count can detect maternal blood in the sample, as fetal white blood cells are primarily leukocytes, while maternal white blood cells are mostly neutrophils.
If amniotic fluid infiltrated the sample, then there would be a reduction in the volume of RBCs, white blood cells, and platelets in the sample.
The most common complication is a hemorrhage of the puncture site and can be especially dangerous when the fetus is younger than 21 weeks.
Severe bleeding may require immediate delivery if the fetus is old enough to survive, or fetal blood volume can be restored with transfusion.
Cord hematoma can cause sudden onset of bradycardia.
Fetomaternal hemorrhage is another complication that occurs when the fetal blood mixes into the maternal blood.
A small fetomaternal hemorrhage could cause an increase in maternal antigens.
A large fetomaternal hemorrhage could cause fetal anemia and death.
Fetal bradycardia may occur most resolve within five minutes.
Infection complication has a low incidence rate.
Preventative antibiotics are used.
Fetal loss may also occur.
Intrahepatic vein fetal blood sampling is an alternative to PUBS.
Intrahepatic vein fetal blood sampling involves inserting a needle
into the intrahepatic part of the umbilical cord in the fetal abdomen: it reduces the chances of contamination of the fetal blood, lowers the risk of fetomaternal hemorrhage, risk of bleeding from the sampling site is reduced, and access to the sampling site is easy regardless of the position of the placenta.
Intrahepatic vein fetal blood sampling is the preferred method of blood sampling With fetal thrombocytopenia.
PUBS is not indicated in every pregnancy.
It is suggested to be done in pregnancy cases in which the blood gas levels and pH would aid in diagnosis of a condition, such as anemia, or delivery plan, or if termination of the pregnancy is being considered.
Umbilical cord blood gas analysis may assist with clinical management and excludes the diagnosis of birth asphyxia in approximately 80% of depressed newborns at term.
Severe fetal growth issues in conjunction with low oxygen in the fetus’ blood and high levels in the mother’s blood are also indications the use of PUBS.
For pregnancies in which genetic abnormalities may be present, PUBS can be used to construct a karyotype, and detect irregular chromosomal patterns.
PUBS allows karyotyping to confirm or detect monosomies, trisomies, or missing portions of chromosomes to give a detailed picture of the severity of the genetic defect as well as predicting developmental future.
PUBS is also indicated in the cases of twins with accumulation of amniotic fluid and substantially different growth rates.
PUBS is also indicated if the fetus is expected to be breaking down red blood cells improperly, and in the alleviation of hydrops fetalis.
Suspicion of fetal infections, such as rubella and toxoplasmosis are indications for PUBS.
The need to supply medicine or blood transfusions to the fetus are indications for the use of PUBS.
Contraindications of PUBS:
PUBS is contraindicated in any fetus under the age of 18 weeks old,
As the umbilical vein from which the blood sample is taken is not very stable, which could lead to excessive bleeding:
these fetuses can be monitored with less invasive procedures and equipment, such as ultrasounds, cardiotocography, or maternal blood tests.
Mothers affected by hepatitis B are not advised to undergo PUBS.
PUBS should not be performed in mothers testing positive for the human immunodeficiency virus (HIV) due to increased risk of fetal contraction.
Fetuses with a single umbilical artery
The most prevalent defect in about 1% of fetuses’ umbilical region is a single umbilical artery.
When a single umbilical artery is found, more tests are run including a detailed ultrasound to detect any other developmental abnormalities.
