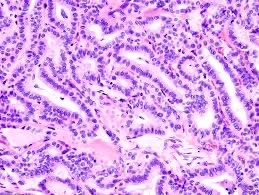
 Rearrangement of the RET protooncogene represents the most common genetic alteration and is regarded as a genetic marker for papillary thyroid cancer(20-40%).
Rearrangement of the RET protooncogene represents the most common genetic alteration and is regarded as a genetic marker for papillary thyroid cancer(20-40%).
Rare in children or young adults in areas not associated with radiation.
Without extracapsular extension there is better than a 95% chance of cure whether treatment with total or hemithyroidectomy.
Can be multifocal in nearly 80% of cases.
More common in women than men 2:1 to 3:1.
Most common type of thyroid carcinoma.
Most important risk factor is radiation.
The exposure to ionizing radiation in childhood has the strongest association who is papillary thyroid cancer.
Detection of small lesion in patient without a family history of thyroid caner or exposure to radiation usually receive intensive treatment for a cancer that is unlikely to cause morbidity or premature mortality.
Studies suggest that patients with small, low risk, thyroid cancer, can be served equally well by surveillance versus immediate surgery (Ho A).
SEER results based on 32 years of data show no significant difference in the death rate from thyroid cancer in patients who did not receive immediate surgery, for low risk disease, than those who did.
Rearrangements of the ret oncogene, which codes for a tyrosine kinase, is found in 10-40% of patients, especially those tumors related to radiation.
Approximately 70% have mutually exclusive gene mutations encoding the growth factor receptors RET or NTRK1 the three isoforms of RAS and BRAF.
Activation of the above stimulates mitogen activated protein kinase (MAPK) signaling which inhibits the expression of thyroid hormone biosynthesis, including Na-iodide symporter and thyroid peroxidase.
40% of patients have the BRAF mutation.
Stratified into low and high-risk groups.
Patients in the low risk group have a favorable prognosis regardless of the treatment.
Patients in high-risk group have a better prognosis with total thyroidectomy and lymph node dissection.
In the past 30 years the rate of thyroidectomy has tripled for thyroid cancers.
Presently there is overtreatment for low risk papillary thyroid cancers, and in patients with no family history or radiation exposure and no evidence of extraglandular involvement, called micropapillary cancers which are less than 20 mm, surgery can be avoided.
In a phase II clinical trial, the BRAF inhibitor vemurafenib demonstrated antitumor activity in patients with BRAFV600E-mutated papillary thyroid cancer who were either tyrosine kinase inhibitor (TKI) treatment naïve or had received prior TKI treatments.
Median progression-free survival (PFS) in treatment-naïve patients treated with vemurafenib was 15.6 months.
Approximately 50% of patients with PTC have tumors with activating
BRAFV600E mutations in papillary cancer of the thyroid is an indicator of poor prognosis.
Oral vemurafenib at 960 mg tablets twice daily.
Across several previous studies, the BRAFV600E mutation has been reported to be associated with several negative prognostic clinicopathologic features as well as an increase in overall mortality in patients with PTC.
25% of patients experience partial response to treatment 75% have stable disease to treatment.
As nearly 50% of patients with PTC in the U.S. are BRAFV600E-mutation positive.
