 1734
1734
A gland about 6 inches long and surrounded by the small intestine, liver and spleen.
Transversely oriented in the retroperitoneum that extends from the “C” loop of the duodenum to the hilum of the spleen.
The organ lies in the retroperitoneum while crossing the body of L1 and L2 along the posterior aspect of the abdominal wall.
Approximately 20 cm in length, and weighs 85-90 gms.
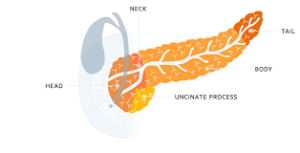
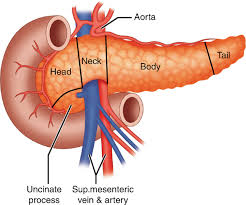
It is divided into five regions, which consist of a head, uncinate process, neck, body, and tail.
The rightmost section, the head of the pancreas, surrounded by the duodenum and delivers pancreatic enzymes directly to the intestines.
To the left is the pancreatic neck, followed by the body and tail.
Uncinate process is part of the gland that bends backwards and underneath the head of the pancreas.
The uncinate lies underneath the body of the pancreas, coming off the posteromedial area of the pancreatic head and curving just posterior to the superior mesenteric artery and vein.
The head of the pancreas is the widest part of the organ, while the uncinate lies underneath the body of the pancreas, coming off the posteromedial area of the pancreatic head and curving just posterior to the superior mesenteric artery and vein.
The head of the pancreas lies just to the right of the superior mesenteric vessels, and it is attached to the second and third portions of the duodenum.
The uncinate is absent in some people, can vary in size and thickness, and has also been noted to encircle the superior mesenteric vessels in others.
The pancreas interacts closely with surrounding blood vessels, delivering insulin and other hormones required for digestion and energy usage.
The neck begins at the passage of the superior mesenteric vessels and spleno-portal vein confluence posterior to the gland.
The neck is the thinnest portion of the pancreas and can be crushed in blunt trauma by being compressed against the second lumbar vertebrae, which sit just posterior to the neck.
The gastroduodenal artery runs in a superior to inferior fashion just to the right of the neck of the pancreas.
The body of the pancreas is covered anteriorly by the omental bursa, which separates the stomach from the pancreas.
The body lies just to the left of the aorta.
The tail of the pancreas is the most mobile aspect of the gland.
The tail usually rests in the hilum of the spleen or just below in the majority of people.
The superior mesenteric artery and vein cross behind the neck of the pancreas and in front of the uncinate process.
The pancreatic duct runs throughout the pancreas and delivers secretions into the duodenum.
Main pancreatic duct, the duct of Wirsung, drains usually into the duodenum at the papilla of Vater.
The majority of pancreatic enzymes are drained through the main pancreatic duct, which then drains out the common channel, which is formed after the meeting of the common bile duct and main pancreatic duct. The common channel length is variable in many patients.
The superior and anterior portions of the pancreatic head are drained by the accessory duct of Santorini, with the remaining portions of the pancreas being drained by the main pancreatic duct of Wirsung.
After the main pancreatic duct and common bile duct join, they enter into the 2nd portion of the duodenum and drain through the ampulla of Vater.
The accessory pancreatic duct, the duct of Santorini, usually drains through a separate minor papilla approximately 2 cm proximal to the papilla of Vater.
The ampulla is surrounded by a muscular ring called the sphincter of Oddi, which controls the flow of bile and pancreatic fluid into the duodenum.
This sphincter is under strict neural and hormonal control.
It is very sensitive to cholecystokinin, which is produced in the duodenum and causes relaxation of the sphincter.
The sphincter of Oddi is under neural and hormonal control.
The common bile duct runs from the gallbladder behind the head of the pancreas to join the pancreatic duct and form the ampulla of Vater at the duodenum.
The vascular supply of the pancreas is is derived from both the celiac artery and the superior mesenteric artery. The common hepatic artery and splenic artery both arise from the celiac trunk.
The common hepatic artery gives rise to the gastroduodenal artery (GDA); the GDA then gives rise to the right gastroepiploic artery after which it continues inferiorly becoming the anterior and posterior superior pancreaticoduodenal arteries.
The superior mesenteric artery supplies both the inferior anterior and posterior pancreaticoduodenal arteries.
These two superior and inferior pancreaticoduodenal arteries supply the pancreatic head, 2nd, and 3rd portions of the duodenum.
The venous drainage of the pancreas usually mirrors the arterial supply.
The veins are usually located anteriorly to the arteries, while the pancreatic ducts are anterior to both arteries and veins.
The venous drainage goes into the superior mesenteric vein, inferior mesenteric vein, splenic vein, or portal vein.
Like the arterial system to the body and tail, three major veins drain these areas.
The inferior pancreatic, caudal, and great pancreatic veins all drain directly into the splenic vein.
These veins are of great importance when a spleen preserving distal pancreatectomy is performed as all these branches must be divided and ligated.
Lymphatic drainage of the pancreas aligns with the vessels supplying the gland.
Two major functions exocrine and endocrine.
The endocrine portion of the pancreas only contributes 1% to 2% of the gland’s function, while the majority of the pancreas is used for exocrine function.
Exocrine function involves the production of digestive enzymes into the pancreatic duct which empties into the duodenum.
The exocrine function is involved with the secretion of enzymes involved in digestion.
The exocrine pancreas has a functional unit called an acinus.
The acinus has zymogen granules that subsequently drain into the main pancreatic duct.
The acinar cells secrete either amylases, lipases, or proteases.
The secretion of these enzymes is due to the parasympathetic system, secretin, and CCK stimulation.
Approximately 50% of the pancreatic acinar cells have to be damaged before there is an effect on their digestion function.
The acinar cell can secrete each of these enzymes, which ultimately appears as an alkaline fluid that is colorless and has no odor.
The pancreas drains between 1 to 2 liters of exocrine fluid per day, which has an alkalotic pH due to the high bicarbonate concentration in the fluid.
As pancreatic stimulation increases, so do the rate of bicarbonate, but chloride concentration decreases.
Endocrine function involves the production of insulin and glucagon hormones which maintain blood sugar levels.
The islets of Langerhans perform the pancreatic endocrine function.
Endocrine pancreas consists of about 1 million clusters of cells, the islets of Langerhans.
These islets consist of 5 cell types- alpha cells that secrete glucagon, beta cells that secrete insulin, delta cells that secrete somatostatin, epsilon cells that secrete ghrelin, and F or PP cells that secrete pancreatic polypeptide.
The hormones are released in a balanced mixture into the portal vein in reaction to changes in the plasma levels.
The majority of the endocrine cells are located in the islet cell periphery, while the beta cells are located in the center and comprise 70% of the islet mass.
Alpha cells are predominantly seen in the islet cells in the superior aspect of the pancreatic head, body, and tail; it accounts for 10% of the islet mass.
Delta cells are like beta cells, which are present in all islets throughout the pancreas.
Delta cells make up only 5% of the islet cell mass.
PP cells are mostly seen in the islets in the pancreas’ head and account for 15% of the islet mass.
Pancreatic secretions range from 600-1500 cc/day.
Pancreatic secretions responsible for most of the digestion of triglycerides in the upper small intestine.
Lipase present in high concentration in pancreatic secretions and its catalytic activity digests dietary fat.
Fat malabsorption that accompanies pancreatic insufficiency is mainly due to lipase deficiency.
Bicarbonate an important component of pancreatic secretions.
Pancreatic enzymes function optimally at a pH of 7-8.
Pancreatic insufficiency can arise from malignancy, chronic pancreatitis, cystic fibrosis, external loss of pancreatic secretions, and gastric acid dumped into the upper gut.
Pancreatic insufficiency can be treated with pancreatic enzyme supplementation or a low fat diet.
Pancreatic enzyme supplementation in pancreatic insufficiency can reverse, but not abolish steatorrhea.
