 Neurolysis is the application of physical or chemical agents to a nerve in order to cause a temporary degeneration of targeted nerve fibers.
Neurolysis is the application of physical or chemical agents to a nerve in order to cause a temporary degeneration of targeted nerve fibers.
When the nerve fibers degenerate, it causes an interruption in the transmission of nerve signals.
It is most commonly and advantageously used to alleviate pain in cancer patients.
The different types of neurolysis: include celiac plexus neurolysis, endoscopic ultrasound guided neurolysis, and lumbar sympathetic neurolysis, chemodenervation and nerve blocks are also associated with neurolysis.
An external neurolysis occurs when scar tissue is removed from around the nerve without entering the nerve itself: A peripheral nerve can be trapped by scarring of surrounding tissue which may lead to potential nerve damage or pain.
Neurolysis is only used when the disease has progressed to a point where no other pain treatments are effective.
A neurolytic agent such as alcohol, phenol, or glycerol is typically injected into the nervous system.
Chemical neurolysis causes fibrosis which then disrupts the sympathetic ganglia, resulting in a reduction of pain signals being transmitted throughout the nerves.
The effects generally last for three to six months.
Celiac plexus neurolysis refers to the chemical ablation of the celiac plexus, which is mainly used to treat pain associated with advanced pancreatic cancer.
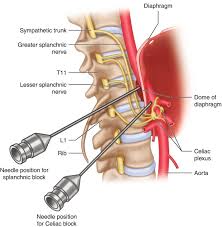
Celiac plexus neurolysis (CPN) can be performed by percutaneous injection either anterior or posterior to the celiac plexus.
CPN is generally performed complementary to nerve blocks, due to the severe pain associated with the injection itself.
CPN and celiac plexus block are different in that celiac plexus neurolysis is permanent ablation whereas celiac plexus block is temporal pain inhibition.
The posterior approaches generally utilize two needles, one at each side of the L1 vertebral body pointing towards the T12 vertebral body.
Endoscopic ultrasound (EUS)-guided neurolysis is a technique that is minimally invasive and can be used to target the celiac plexus, the celiac ganglion, or the broad plexus in the treatment of pancreatic cancer-associated pain.
EUS-guided celiac plexus neurolysis (EUS-CPN) is performed via an echoendoscope passed through the mouth into the esophagus to the gastroesophageal junction.
EUS imaging allows the doctor to visualize the aorta, which can then be traced to the origin of the celiac artery, where neurolysis is then performed with a spray needle that disperses a neurolytic agent, such as alcohol or phenol, into the celiac plexus.
Lumbar sympathetic neurolysis is used on patients with ischemic rest pain, with repairable arterial occlusive disease.
Peripheral neuralgia or vasospastic disorders can receive lumbar sympathetic neurolysis for pain treatment.
The chemicals used for neurolysis of the nerves cause destructive fibrosis and cause a disruption of the sympathetic ganglia.
Lumbar sympathetic neurolysis chemicals alter ischemic rest pain transmission by changing norepinephrine and catecholamine levels or by disturbing afferent fibers.
Lumbar sympathetic neurolysis is performed by using absolute alcohol, phenol, radiofrequency or laser ablation.
Fluoroscopy or CT guidance is used.
Complications of this procedure include nerve root injury, bleeding, and paralysis.
Complications are diminished when using radiofrequency or laser ablation techniques in comparison to the injection of alcohol or phenol.
Approximately two-thirds of patients achieve pain relief with minimal complications,
Chemodenervation is a process used to manage focal muscle overactivity through the use of either phenol, alcohol, or botulinum toxins (BoNTs).
Chemodenervation is used as a complement to neurolysis.
The agent of choice is injected into the muscle fibers as opposed to nerve tissue to dull the neuronal signaling within the muscles.
Chemodenervation is commonly used in the field of medicine to treat various medical conditions, such as muscle spasms, dystonia, and certain types of wrinkles.
The most well-known form of chemodenervation is the use of botulinum toxin, commonly referred to as Botox.
Botox injections temporarily paralyze or weaken specific muscles by blocking the release of acetylcholine, a neurotransmitter that stimulates muscle contractions.
This can be beneficial in treating conditions like muscle spasms or reducing the appearance of wrinkles.
