 Microscopic colitis (MC) refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis.
Microscopic colitis (MC) refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis.
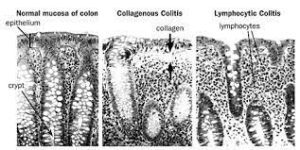
Both conditions are characterized by the presence of chronic non-bloody watery diarrhea, normal appearances on colonoscopy and characteristic histopathology findings of inflammatory cells.
Incidence and prevalence of microscopic colitis nears those of ulcerative colitis and Crohn’s disease.
Studies in North America found incidence rates of 7.1 per 100,000 person-years and 12.6 per 100,000 person-years for collagenous colitis for lymphocytic colitis, respectively.
Prevalence has been estimated as 103 cases per 100,000 persons.
Patients are characteristically, though not exclusively, middle-aged females.
The average age of diagnosis is 65 but 25% of cases are diagnosed below the age of 45.
Differential diagnosis;
Bile acid diarrhea, celiac disease, lactose malabsorption, Crohn’s disease, ulcerative colitis, infectious colitis.
103 cases per 100,000 persons
The main symptom is persistent non-bloody watery diarrhea, which may be profuse.
People may also experience abdominal pain, fecal incontinence, and unintentional weight loss.
Microscopic colitis is the diagnosis in around 10% of cases investigated for chronic non-bloody diarrhea.
Associated with higher incidence of autoimmune diseases, for example arthritis, Sjögren’s syndrome, thyroid disorders, and celiac disease, has been reported in people with microscopic colitis.
Microscopic colitis can cause nocturnal diarrhea even if fasting.
The condition inflames the large intestine at a microscopic level.
Associations with various drugs: proton pump inhibitors, H2 blockers, selective serotonin reuptake inhibitors (SSRIs), and non-steroidal anti-inflammatory drugs (NSAIDs).
Bile acid diarrhea is found in 41% of patients with collagenous colitis and 29% with lymphocytic colitis.
Cigarette smoking has been identified as a significant risk factor of microscopic colitis.
Colonoscopic appearances are normal or near normal.
As bowel changes are often patchy, a full colonoscopy is necessary for diagnosis.
Multiple colonic biopsies are required to make the diagnosis.
Histological features of colonic biopsies indicating microscopic colitis are: greater than 20 intraepithelial lymphocytes per 100 epithelial cells and, 10-20 μm of a thickened subepithelial collagen band in collagenous colitis, and inflammation of the lamina propria, with mainly mononuclear cells, in collagenous colitis.
The process is characterized by an increase in inflammatory cells, particularly lymphocytes, with an otherwise normal appearance and architecture of the colon on biopsy.
Inflammatory cells are involved in both on the surface epithelium of the colon and in its lamina propria.
The two types of microscopic colitis share many features: epidemiology, risk factors and, response to therapy suggesting that they are actually subtypes of the same disease.
Differential diagnosis: bile acid diarrhea, lactose malabsorption, celiac disease, Crohn’s disease, ulcerative colitis, and infectious colitis.
Treatment
Lymphocytic and collagenous microscopic colitis respond well to budesonide, a glucocorticoid.
Relapse occurs frequently after withdrawal of therapy.
Other agents used include: antidiarrheals, bismuth subsalicylate, mesalazine/mesalamine, alone or in combination with cholestyramine, systemic corticosteroids, cholestyramine, immunomodulators, and probiotics.
For refractory MC: Anti-TNF inhibitors. split ileostomy, diverting ileostomy, and subtotal colectomy are options for management of steroid-dependent or refractory microscopic colitis.
Surgery is considered for patients with severe, unresponsive microscopic colitis.
The prognosis for lymphocytic colitis and collagenous colitis is good, and both conditions are considered to be benign.
The majority of people recover from their diarrhea, and their histological abnormalities resolve.
Relapses commonly occur if maintenance treatment is not continued.
