 Following transition from a reproductive, premenopausal status marked by regular ovulation and cyclic menstruation to a postmenopausal period noted by amenorrhea.
Following transition from a reproductive, premenopausal status marked by regular ovulation and cyclic menstruation to a postmenopausal period noted by amenorrhea.
Permanent cessation of menstruation that results from loss of ovarian function.
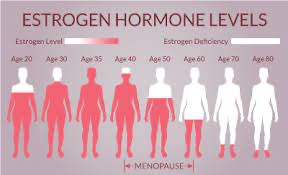
Most women experience menopause as a natural life course event due to permanent loss of ovarian follicular activity, and related estrogen production.
Premature hypoestrogenism due to primary ovarian insufficiency, surgical, oophorectomy, or medication induced menopause refers to menopause before the age of 40 years.
The surgical menopause refers to bilateral oophorectomy that is performed prior to natural menopause.
Hysterectomy in the absence of bilateral oophorectomy, does not constitute surgical menopause.
Women spend less than 40% of their lifespan in the post menopausal stage.
A discrete event marked by the permanent cessation of ovarian function, diagnosed after 12 months of amenorrhea.
An occult event that is only evident after 12 consecutive months of amenorrhea.
Whether natural or induced the proximate cause of menopause is ovarian primordial follicle reserve depletion.
Can occur naturally, surgically or from medical intervention.
Perimenopause and menopause means that bone loss starts outpacing new bone building.
Women can lose up to 20% of their bone density after menopause.
In menstruating women, cessation of menses for 12 months is the threshold for menopause.
The average age of menopause is approximately 51 years.
Natural menopause occurs within the ages of 45 years and 56 years in 90% of women.
Almost all women experience at a median age of 47 years early phase of the menopausal transition presented when a woman with a previously regular cycle experiences irregularity in her intermenstrual interval of seven days or more.
Menopausal transition is divided into periods.
The early menopausal transition begins when the length of the menstrual cycle becomes variable of seven day or greater difference in the length of consecutive menstrual cycles, and the late menopausal transition is characterized by amenorrhea for 60 days or longer.
Perimenopause is composed of the menopausal transition, and the 12 months following the final menstrual period.
Age at onset of menopausal transition is predictive of its duration, with women who enter the transition at early ages having a longer and more symptomatic transitions.
Women entering the transitions at older ages may have a brief transition stage or even skip stages and progressed directly from regular cycles to permanent amenorrhea.
At a median age of 49 years, the next menstrual marker is amenorrhea lasting more than 60 days defining the late transition with a 95% probability that the final menstrual period will occur within four years.
It specifically defines a point in time 12 months after a woman has her last period, according to the National Institute on Aging (NIA).
Premature menopause of less than 40 years, either natural or surgical is associated with an elevated risk of cardiovascular disease.
Women with spontaneous spontaneous primary ovarian insufficiency are at increased risk for impaired endothelial function and early onset of ischemic heart disease.
A decrease in estrogen has been linked to a less active metabolism.
Fluctuating mood is common in perimenopause, probably because hormone levels that keep changing before they finally settle down after menopause.
Mood swings before menopause may also be more pronounced in women who have bad premenstrual syndrome earlier in their lives, or who have a history of depression.
Sleeping difficulties are common among perimenopausal and menopausal women.
Sleeping difficulties affect as many as half of such women, aged 40 to 64.
Sleeping difficulties include: poor sleep quality, insomnia due to hot flashes and night sweats.
Genitourinary symptoms include dyspareunia, vaginal dryness, vaginal burning, vaginal pruritus, dysuria, urinary urgency, and recurrent urinary tract infections.
The genitourinary symptoms of menopause are experienced by approximately 45 to 70% 77% of women, generally worsen over time, and persist indefinitely.
During menopause transition, approximately 50 to 75% of women begin having vasomotor symptoms and more than 50% begin having genitourinary symptoms.
More than 50% of women experience frequent vasomotor symptoms for six or more days in the previous two weeks.
Frequent vasomotor symptoms last more than seven years in approximately 50% of women.
The median age of the final menstrual period for US women is 52.5 years, with most women becoming menopausal between ages 47-54 years.
Up to 10% of women undergo menopause before age 45 years, and 1% experience menopause before age 40.
BMI, education, and social stressors influence the age of menopause.
Follicle oocyte reserve is established in utero and cannot be replenished.
Estradiol levels are typically less than 30 pg/mL in the postmenopausal state.
Elevated FSH level and reduced estradiol levels generally confirm the clinical diagnosis of menopause.
FSH is produced by the pituitary, partially in response to gonadotropin releasing hormone and partially in response to pituitary activin.
FSH is also going to do inhibitory control by estradiol and the inhibiting peptides A and B in the follicular phase of the cycle.
Inhibin A is the product primarily of the corpus luteum and present and largely contributes FSH suppression during pregnancy.
FSH is an indirect measure of follicle reserve that requires an intact hypothalamus pituitary axis for clinically meaningful interpretation.
FSH fluctuates almost tenfold over the course of a menstrual cycle and should be measured, typically within five days of the onset of menses, when it is most consistent and at its highest to have the ability to predict the final menstrual period.
FSH fluctuates almost 10 times over the course of a normal menstrual cycle.
FSH levels determined within the first five days of onset of menstrual bleeding are commonly used to project ovarian response to fertility treatments.
FSH levels are typically measured within five days of the onset of menses, when is most consistent and its highest.
After menopause circulating estradiol is derived from estrone, which is converted in adipose tissue from adrenal androstenedione.
It provides a more direct indicator of the ovarian oocyte reserve.
Levels peak in the mid-20s, and then declines progressively in concert with follicle loss.
It is not produced by primordial follicles in the ovary, and it is only secreted once primordial follicle growth activation has occurred, but very low levels suggest of impending menopause.
Female fertility is very low for approximately a decade before menopause and is declining during the during the 30s.
The measurement of circulating sex steroids and pituitary gonadotrophins allows assessment of ovulatory function and diagnosis of the main relevant disorders of the ovary.
Ovarian and pituitary hormones do not reflect the activity of the great majority of follicles within the ovary, whose growth is necessary to support ovulation and fertility.
Smaller follicles present in the ovary are determinants of reproductive lifespan and age at menopause.
The transition to menopause is noted by changes in the menstrual cycle with variation in the duration and degree of menstrual flow.
Transition usually begins in mid to late 40s and lasts about 4 years.
Median age occurs at 51 years.
Early in the menopausal transition period cycles are erratic and may be missed.
After 12 months of amenorrhea menopause can be defined, retrospectively.
The risk of premature or early menopause is higher among women who began having menstrual periods at a young age and did not have children.
Premature menopause is associated with an increased risk of coronary artery disease, less consistently, with increased risk of stroke, increased risk of heart failure, increased risk of aortic stenosis, mitral regurgitation, atrial fibrillation , ischemic stroke, peripheral artery disease, and venous thromboembolism.
Early menopause may be linked to Alzheimer’s disease.
Some women complain of memory lapses and difficulty finding the right word, during and after menopause: The evidence linking this specifically to hormonal changes is weak.
In women who do have noticeable cognitive impairment it is related to other menopausal symptoms such as sleep deprivation.
Early menopause at age 40 or younger is associated with lasting negative effects in cognitive function.
Early menopause may be linked to Alzheimer’s disease.
More women than men develop Alzheimer’s as they age, and the decline in estrogen at menopause may leave women’s brains more vulnerable to the disease.
Cognitive problems reported including difficulty retrieving words or numbers, forgetting the purpose of a behavior, losing one’s train of thought, and overlooking appointments.
LH levels higher in perimenopausal women than in younger women.
Level of FSH begins to increase but is generally in the normal range during early menopause.
As transition occurs estrogen levels fall markedly and levels of FSH increase.
Ovulation does not occur after menopause is complete.
After menopause the ovaries do not produce estradiol or progesterone, but continue to produce testosterone.
A small amount of estrogen is produced by the metabolism of adrenal steroids by conversion to estradiol in peripheral fat tissue.
During perimenopausal transition circulating estrogen levels are equivalent or higher than levels in younger women.
There is a decreases in estrogen sensitivity in the menopausal transition period.
Cigarette smokers undergo process about 2 years earlier than nonsmokers.
Change in hormonal milieu associated with perimenopause and menopause can lead to symptoms of hot flashes, night sweats, emotional lability, poor concentration, and sleep disturbance.
Hot flashes and sleep disturbances more common in perimenopausal than in postmenopausal women.
Decrease sensitivity to estrogen during the menopausal period.
Most women enter menopause in their late 40’s or early 50’s.
The first menstrual changes of menopause are shortening of the cycles followed by erratic cycle length.
Hot flashes often start while the patient is still having menstrual cycles.
Cognitive changes, insomnia, moodiness and decreased libido common problems.
Urogenital symptoms usually occur late in menopausal transition.
With surgical, chemotherapy or radiation induced menopause patients are more likely to experience severe symptoms.
Risk of premature menopause with multiple agent chemotherapy approximately 53-89%.
More than 1 in 3 women are postmenopausal and cardiovascular disease is the number one cause of death in postmenopausal women.
Alters lipoprotein levels, most frequently in the form of an increase low-density lipoprotein (LDL) cholesterol concentrations.
Results in central fat distribution.
Age and BMI matched women, those who are postmenopausal tend to have a greater percentage of body fat in the central distribution as compared with premenopausal women.
Visceral fat deposits may increase 15 – 20% of the total body fat compared with 5 – 8% in the premenopausal state.
More than one third of women’s lives will occur after cessation of menses.
LH levels higher in perimenopausal women than in younger women.
Level of FSH begins to increase but is generally in the normal range during early menopause.
As transition occurs estrogen levels fall markedly and levels of FSH increase.
Ovulation does not occur after menopause is complete.
After menopause the ovaries do not produce estradiol or progesterone, but continue to produce testosterone.
A small amount of estrogen is produced by the metabolism of adrenal steroids by conversion to estradiol in peripheral fat tissue.
During perimenopausal transition circulating estrogen levels are equivalent or higher than levels in younger women.
There is a decreases in estrogen sensitivity in the menopausal transition period.
Cigarette smokers undergo process about 2 years earlier than nonsmokers.
Change in hormonal milieu associated with perimenopause and menopause can lead to symptoms of hot flashes, night sweats, emotional lability, poor concentration, and sleep disturbance.
Hot flashes and sleep disturbances more common in perimenopausal than in postmenopausal women.
75% or more will experience bothersome vasomotor symptoms.
Costs associated with untreated vasomotor symptoms are estimated nearly $400,000,000 annually.
Decrease sensitivity to estrogen during the menopausal period.
Most women enter menopause in their late 40’s or early 50’s.
The first menstrual changes of menopause are shortening of the cycles followed by erratic cycle length.
Hot flashes often start while the patient is still having menstrual cycles.
Cognitive changes, insomnia, moodiness and decreased libido common problems.
Urogenital symptoms usually occur late in menopausal transition.
There is a range of bladder and genital changes and symptoms that are associated with menopause-the genitourinary syndrome of menopause.
This syndrome includes vulva atrophy, vaginal dryness, and in some cases bladder function changes.
Estrogen receptors on the bladder and urethra help with bladder and urethral functions.
Bladder problems often consist of stress incontinence, which may be more noticeable with multiple vaginal, birthings.
Women’s risk of heart disease increases after menopause, and the decline in estrogen likely plays a role.
Estrogen usually helps keep blood vessels flexible, improving circulation.
Menopause does not cause heart disease, as other contributing factors also change at this time in life:lipids, hypertension, inactivity, and lifestyle events.
With surgical, chemotherapy or radiation induced menopause patients are more likely to experience severe symptoms.
Risk of premature menopause with multiple agent chemotherapy approximately 53-89%.
More than 1 in 3 women are postmenopausal and cardiovascular disease is the number one cause of death in postmenopausal women.
Sleep disturbances are common in menopause.
The pattern of menstrual periods changes during perimenopause.
Cycles during perimenopause can’t become longer or shorter, and sometimes, people may skip periods altogether.
The
When approaching menopause, hormonal shifts cause their bodies to ovulate less frequently.
When the ovary does not release an egg, the uterus lining does not shed, and the person does not have a period.
The most common shift in the menstrual cycle is that a person begins to have fewer monthly periods.
Because ovulation is not occurring cyclically during perimenopause, the body produces smaller amounts of progesterone causing the lining of the uterus to build up for longer than usual, which makes periods less frequent and heavier.
Because of these hormonal fluctuations, people may notice the following occurs because people are ovulating less often.
Longer, heavier periods happens because the lining of the uterus has time to grow thicker and takes longer to shed.
Lighter periods may be experienced lighter when estrogen levels are low.
This is because estrogen increases the thickness of the uterus lining.
People may have irregular periods, spotting between periods, or both, when the uterus lining grows thicker than usual.
The time between monthly periods can also vary greatly.
Some people’s periods may change unpredictably from month to month.
Over time, perimenopause will cause a person’s periods to become less frequent and eventually to stop altogether.
The transition into menopause as complete when an individual has gone 1 year without a period.
After 1 year, people should talk to their doctor about any vaginal bleeding.
Eating a diet rich in soy products may help people regulate their hormones, and can reduce the number of menopause symptoms a person experiences.
Because most people still have periods during perimenopause, it is still possible to get pregnant during this time.
The use of birth control pills, or hormonal contraceptives, can mask some of the symptoms of menopause, making it difficult for a person to know if they are going through menopause.
The time between monthly periods can also vary greatly. Some people’s periods may change unpredictably from month to month. For example, their period may be heavy one month and absent the next.
Perimenopause is not a disease and does not require treatment.
People going through perimenopause should see a doctor if:
they experience side effects associated with hormone treatments
they bleed after 1 year without a period
they experience bleeding that is very heavy, very painful, or that soaks through more than a pad or tampon an hour
hormone therapy stops helping with perimenopause symptoms
they experience pain or bleeding during or after sex.
