
 Tumors that grow within the pancreatic ducts (intraductal) characterized by the production of thick mucin.
Tumors that grow within the pancreatic ducts (intraductal) characterized by the production of thick mucin.
Some of these lesions progress to invasive cancer.
Intraductal papillary mucinous neoplasms represent an opportunity to treat a pancreatic tumor before it develops.
2.6 out of every 100 individuals examined by CT of the abdomen have a pancreatic cyst, and most of these are intraductal papillary mucinous neoplasms.
Strong correlation between pancreatic cysts and age with no cysts among patients less than 40 years of age, and 8.7 percent of the patients age 80 to 89 years have a pancreatic cyst.
Arise from pancreatic ducts lined with mucin secreting columnar cells.
Intraductal papillary mucinous neoplasms may be associated with an invasive cancer or not.
95% of IPMN resected without an invasive pancreatic cancer are cured.
Intraductal papillary mucinous neoplasms are subcategorized into three groups:with low-grade dysplasia, IPMN with moderate dysplasia, and IPMN with high-grade dysplasia.
The lesion may originate in the main pancreatic duct or from a branch duct, with the latter lesions being less aggressive.
Patients may present with abdominal pain, nausea and vomiting, weight loss, possibly jaundiced or with pancreatitis, but it is increasingly common to diagnose these individuals in an asymptomatic state as the lesion is often found incidentally.
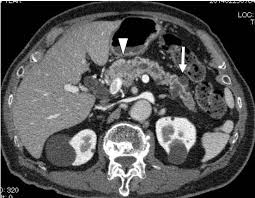
Diagnosis can be confirmed by imaging studies to include computerized tomography (CT), endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP) revealing dilatation of the pancreatic duct or one its branches.
In some cases a fine needle aspiration (FNA) biopsy using endoscopic ultrasound, CT scan or abdominal ultrasound can be obtained to confirm the diagnosis.
As many as 70% of main duct type intraductal papillary mucinous neoplasms harbor high-grade dysplasia or an invasive cancer.
Main pancreatic duct type IPMNs are significant lesions, and should be resected.
IPMNs of the tail of the pancreas are usually resected with a distal pancreatectomy, while lesions in the head and body of the pancreas require a pancreaticoduodenectomy.
The management of branch duct IPMNs is more complicated since many of these lesions are not aggressive and surgical risks outweigh the benefits of resection.
Asymptomatic patients with a branch duct intraductal papillary mucinous lesions less than 3 cm in size, not associated with dilatation of the main pancreatic duct, and does not contain a solid mas, can be followed without surgery.
Branch duct IPMNs not surgically resected should be monitored radiographically for growth or the development of a mass which are indication to surgically remove the IPMN.
Imaging studies to monitor branch duct IPMNs for growth include CT, endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP).
Smaller branch duct IPMNs less than 1 cm in diameter can be followed with an annual imaging studies and larger IPMNs should have review frequently as every three months.
These lesions can be multiple and patients remain at risk for developing a second lesion.
Patients have a slightly increased risk of developing tumors of the colon and rectum.
Circulating epithelial cells can be detected from patients with these lesions in up to 33% of patients (Rhim AD).
Circulating epithelial cells emerge early during tumorigenesis, and only after malignant transformation do these circulating epithelial cells become circulating tumor cells
