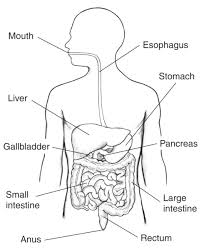
The digestive system consists of the gastrointestinal tract plus the accessory organs of digestion: the tongue, salivary glands, pancreas, liver, and gallbladder.
Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body.
The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.
The first stage of digestion is the cephalic phase.
This stage includes the mechanical breakdown of food by chewing, and the chemical breakdown by digestive enzymes, that takes place in the mouth.
Saliva contains the digestive enzymes amylase, and lingual lipase, secreted by the salivary and serous glands on the tongue.
Chewing, mixes the food with saliva, and begins the mechanical process of digestion.
This produces a bolus which is swallowed down the esophagus to enter the stomach.
Secretions from gastric glands respond to the sight and smell of food.
The second stage, the gastric phase, occurs in the stomach, where the food is further broken down by mixing with gastric acid until it passes into the duodenum, the first part of the small intestine.
The third stage, the intestinal phase, begins in the duodenum, where the partially digested food is mixed with a number of enzymes produced by the pancreas.
Digestion is assisted by the chewing of food carried out by the muscles of mastication, the tongue, and the teeth, and also by the contractions of peristalsis, and segmentation.
Gastric acid, and mucus in the stomach, are essential for the continuation of digestion.
Peristalsis, the rhythmic contraction of muscles that begins in the esophagus and continues along the wall of the stomach and the rest of the gastrointestinal tract results in the production of chyme which when fully broken down in the small intestine is absorbed as chyle into the lymphatic system.
Chyme is the pulpy acidic fluid which passes from the stomach to the small intestine, consisting of gastric juices and partly digested food.
Chyle is a milky fluid consisting of fat droplets and lymph-It drains from the lacteals of the small intestine into the lymphatic system during digestion.
Most of the digestion of food takes place in the small intestine.
Water and some minerals are reabsorbed back into the blood in the colon of the large intestine.
Feces, the waste products of digestion are defecated from the rectum via the anus.
There are organs and other components involved in the digestion of food.
The organs known as the accessory digestive organs are the liver, gall bladder and pancreas.
Other components include the mouth, salivary glands, tongue, teeth and epiglottis.
The largest structure of the digestive system is the gastrointestinal tract (GI tract).
The GITMstarts at the mouth and ends at the anus, covering a distance of about nine meters.
Within the stomach mucosa there are millions of embedded gastric glands, whose secretions are vital to the functioning of the organ.
Most of the digestion of food takes place in the small intestine which is the longest part of the GI tract.
The largest part of the GI tract is the colon or large intestine.
Water is absorbed here and the remaining waste matter is stored prior to defecation.
Specialized cells of the GI tract: various cells of the gastric glands, taste cells, pancreatic duct cells, enterocytes and microfold cells.
Some parts of the digestive system are also part of the excretory system, including the large intestine.
The mouth the first part the digestive system is equipped with several structures that begin the first processes of digestion, including salivary glands, teeth and the tongue.
The mouth consists of two regions; the vestibule and the oral cavity proper.
The vestibule is the area between the teeth, lips and cheeks, and the rest is the oral cavity proper.
The oral cavity is lined with oral mucosa, a mucous membrane that produces a lubricating mucus.
Mucous membranes vary in structure in the different regions of the body.
All mucous membranes produce a lubricating mucus, which is either secreted by surface cells or more usually by underlying glands.
The mucous membrane in the mouth has a thin mucosa which lines the bases of the teeth.
The main component of mucus is a glycoprotein called mucin and the type secreted varies according to the region involved.
Mucin is viscous, clear, and clinging.
Underlying the mucous membrane in the mouth is a thin layer of smooth muscle tissue, and it has a loose connection to the membrane giving it elasticity.
Oral mm covers the cheeks, inner surfaces of the lips, and floor of the mouth, and the mucin produced is highly protective against tooth decay.
The roof of the mouth is termed the palate and it separates the oral cavity from the nasal cavity.
The palate is hard at the front of the mouth since the overlying mucosa is covering a plate of bone
The palate is softer and more pliable at the back being made of muscle and connective tissue, and it can move to swallow food and liquids.
The soft palate ends at the uvula.
The surface of the hard palate allows for the pressure needed in eating food, and to leave the nasal passage clear.
The opening between the lips is termed the oral fissure/
The opening into the throat is called the fauces.
At either side of the soft palate are the palatoglossus muscles which also reach into regions of the tongue.
The palatoglossus muscles raise the back of the tongue and also close both sides of the fauces to enable food to be swallowed.
Mucus helps in the mastication of food in its ability to soften and collect the food in the formation of the bolus.
There are three pairs of main salivary glands and between 800 and 1,000 minor salivary glands, all of which mainly serve the digestive process.
Salivary glands play an important role in the maintenance of dental health and general mouth lubrication, without which speech would be impossible.
The main salivary glands are all exocrine glands, secreting via ducts, terminating in the mouth.
The largest of these are the parotid glands—their secretion is mainly serous.
The next pair are underneath the jaw, the submandibular glands, these produce both serous fluid and mucus.
The serous fluid is produced by serous glands in these salivary glands which also produce lingual lipase.
They produce about 70% of the oral cavity saliva.
The third pair are the sublingual glands located underneath the tongue and their secretion is mainly mucous with a small percentage of saliva.
Within the oral mucosa, and also on the tongue, palates, and floor of the mouth, are the minor salivary glands; their secretions are mainly mucous and they are innervated by the facial nerve (CN7).
The minor salivary glands secrete amylase a first stage in the breakdown of food acting on the carbohydrate in the food to transform the starch content into maltose.
Serous glands on the surface of the tongue that encircle taste buds on the back part of the tongue and these also produce lingual lipase.
Lipase is a digestive enzyme that catalyses the hydrolysis of fats.
Serous glands on the surface of the tongue (Von Ebner’s glands) secrete histatins which offer a defense against microbes in food, when they make contact with these glands on the tongue tissue.
Sensory information stimulates the secretion of saliva providing the necessary fluid for the tongue to work with and also to ease swallowing of the food.
Saliva moistens and softens food, and along with the chewing action of the teeth, transforms the food into a smooth bolus.
The bolus is helped by the lubrication provided by the saliva in its passage from the mouth into the esophagus.
In saliva are the digestive enzymes amylase and lipase.
Amylase starts to work on the starch in carbohydrates, breaking it down into the simple sugars of maltose and dextrose that can be further broken down in the small intestine.
Saliva in the mouth can account for 30% of this initial starch digestion.
Lipase starts to work on breaking down fats.
Lipase is further produced in the pancreas where it is released to continue this digestion of fats.
The presence of salivary lipase is of prime importance in young babies whose pancreatic lipase has yet to be developed.
Saliva has a cleansing action for the teeth and mouth.
Saliva has an immunological role in supplying antibodies to the system, such as immunoglobulin A, preventing infections of the salivary glands, importantly that of parotitis.
Saliva also contains a glycoprotein haptocorrin which is a binding protein to vitamin B12 to carry it safely through the acidic content of the stomach.
When it reaches the duodenum, pancreatic enzymes break down the glycoprotein and free the vitamin which then binds with intrinsic factor.
The tongue is a fleshy and muscular sensory organ, and provides the first sensory information of the digestive system via the taste buds in the papillae on its surface.
The tongue manipulates the food in the mouth which stimulates the secretion of saliva from the salivary glands.
The liquid quality of the saliva softens the food and its enzyme content will start to break down the food as it is still in the mouth.
The first part of the food to be broken down is the starch by the enzyme amylase in the saliva.
The tongue is attached to the floor of the mouth by a ligamentous band called the frenum and this gives it great mobility for the manipulation of food, and speech.
The range of manipulation of then tongue is optimally controlled by the action of several muscles and limited in its external range by the stretch of the frenum.
The tongue’s two sets of muscles, are four intrinsic muscles that originate in the tongue and are involved with its shaping, and four extrinsic muscles originating in bone that are involved with its movement.
Taste is a form of chemoreception that takes place in the specialized taste receptors, contained in structures called taste buds in the mouth.
Taste buds are mainly on the upper surface of the tongue.
The function of taste perception is vital to help prevent harmful or rotten foods from being consumed.
Taste buds are also present on the epiglottis and upper part of the esophagus.
The taste buds are innervated by a branch of the facial nerve the chorda tympani, and the glossopharyngeal nerve.
Taste messages are sent via these cranial nerves to the brain.
The brain can distinguish between the chemical qualities of the food.
The five basic tastes are referred to as those of saltiness, sourness, bitterness, sweetness, and umami.
The detection of saltiness and sourness enables the control of salt and acid balance.
The detection of bitterness warns of poisons, as many of a plant’s defences are of poisonous compounds that are bitter.
Sweetness guides to those foods that will supply energy; the initial breakdown of the energy-giving carbohydrates by salivary amylase creates the taste of sweetness since simple sugars are the first result.
The taste of umami is thought to signal protein-rich food.
Sour tastes are acidic which is often found in bad food.
Olfactory receptors are located on cell surfaces in the nose which bind to chemicals enabling the detection of smells.
Signals from taste receptors work together with those from the nose, to form an idea of complex food flavors.
Teeth are complex structures made of made of a bone-like material called dentin, which is covered by the hardest tissue in the body—enamel.
Teeth’s different shapes deal with different aspects of mastication employed in tearing and chewing pieces of food into smaller and smaller pieces.
The smaller pieces of food result in a much larger surface area for the action of digestive enzymes.
The teeth are named after their roles in the process of mastication.
Incisors are used for cutting or biting off pieces of food;
Canines, are used for tearing,
Premolars and molars are used for chewing and grinding.
Mastication of the food with the help of saliva and mucus results in the formation of a soft bolus which can then be swallowed to make its way down the upper gastrointestinal tract to the stomach.
The digestive enzymes in saliva also help in keeping the teeth clean by breaking down any lodged food particles.
The epiglottis is a flap of elastic cartilage attached to the entrance of the larynx.
The epiglottis is covered with a mucous membrane and there are taste buds on its lingual surface which faces into the mouth.
Its laryngeal surface faces into the larynx.
The epiglottis functions to guard the entrance of the glottis, the opening between the vocal folds.
The epiglottis normally pointed upward during breathing with its underside functioning as part of the pharynx.
During swallowing, the epiglottis folds down to a more horizontal position, with its upper side functioning as part of the pharynx, preventing food from going into the trachea and instead directs it to the esophagus, which is behind.
Upon swallowing, the backward motion of the tongue forces the epiglottis over the glottis’ opening to prevent any food that is being swallowed from entering the larynx which leads to the lungs; the larynx is also pulled upwards to assist this process.
Stimulation of the larynx by ingested matter produces a strong cough reflex in order to protect the lungs.
The pharynx is a part of the conducting zone of the respiratory system and also a part of the digestive system.
The pharynx is a part of the throat immediately behind the nasal cavity at the back of the mouth and above the esophagus and larynx.
The pharynx is made up of three parts.
The lower two parts—the oropharynx and the laryngopharynx are involved in the digestive system.
The laryngopharynx connects to the esophagus and it serves as a passageway for both air and food.
Air enters the larynx anteriorly but anything swallowed has priority and the passage of air is temporarily blocked.
The pharynx is innervated by the pharyngeal plexus of the vagus nerve.
Muscles in the pharynx push the food into the esophagus. The pharynx joins the esophagus at the oesophageal inlet which is located behind the cricoid cartilage.
The esophagus, is commonly known as the foodpipe.
It consists of a muscular tube through which food passes from the pharynx to the stomach.
The esophagus is continuous with the laryngopharynx.
It passes through the posterior mediastinum in the thorax and enters the stomach through a hole in the thoracic diaphragm—the esophageal hiatus, at the level of the tenth thoracic vertebra (T10).
The esophageal length averages 25 cm, varying with an individual’s height.
It is divided into cervical, thoracic and abdominal parts.
The pharynx joins the esophagus at the esophageal inlet which is behind the cricoid cartilage.
At rest the esophagus is closed at both ends, by the upper and lower esophageal sphincters.
The opening of the upper sphincter is triggered by the swallowing reflex so that food is allowed through.
The sphincter also prevents back flow from the esophagus into the pharynx.
The esophagus has a mucous membrane and the protective epithelium is continuously replaced.
With swallowing, food passes from the mouth through the pharynx into the esophagus, and the epiglottis folds down to a more horizontal position to direct the food into the esophagus, and away from the trachea.
Food in the esophagus, travels a bolus down to the stomach via rhythmic contraction and relaxation of muscles (peristalsis)>
The lower esophageal sphincter is a muscular sphincter surrounding the lower part of the esophagus, at the gastroesophageal junction.
The lower esophageal sphincter remains constricted at all times other than during swallowing and vomiting to prevent the contents of the stomach from entering the esophagus.
Because the esophagus does not have the same protection from acid as the stomach, any failure of this sphincter can lead to heartburn.
The muscular diaphragm separates the thoracic cavity from the abdominal cavity.
The suspensory muscle attaches the ascending duodenum to the diaphragm, helping the digestive system in that its attachment offers a wider angle to the duodenojejunal flexure for the easier passage of digesting material.
The diaphragm also anchors the liver at its bare area.
The esophagus enters the abdomen through a hole in the diaphragm at the level of T10.
The stomach is a major organ of the gastrointestinal tract and digestive system.
A J-shaped organ joined to the esophagus at its upper end and to the duodenum at its lower end.
Gastric acid produced in the stomach has a vital role in the digestive process, and mainly contains hydrochloric acid and sodium chloride.
A peptide hormone, gastrin, produced by G cells in the gastric glands, stimulates the production of gastric juice which activates the digestive enzymes.
Pepsinogen is a precursor enzyme (a zymogen) produced by the gastric chief cells, and gastric acid activates this to the enzyme pepsin which begins the digestion of proteins.
Because gastric and pepsinogen chemicals can damage the stomach wall, mucus is secreted by innumerable gastric glands in the stomach, providing a slimy protective layer against the damaging effects of the chemicals on the inner layers of the stomach.
Mechanical churning occurs through peristalsis, waves of muscular contractions, that move along the stomach wall.
Peristalsis allows the mass of food to mix with the digestive enzymes.
Gastric lipase is secreted by the chief cells in the fundic glands of the gastric mucosa of the stomach, and is is an acidic lipase: it contrasts with the alkaline pancreatic lipase.
Gastric lipase breaks down fats to some degree though is not as efficient as the pancreatic lipase.
The pylorus is the lowest section of the stomach which attaches to the duodenum via the pyloric canal.
The pylorus contains glands which secrete digestive enzymes including gastrin.
After an hour or two, a thick semi-liquid called chyme is produced in the stomach.
When the pyloric sphincter, or valve opens, the chyme enters the duodenum when the pyloric sphincter where it mixes further with digestive enzymes from the pancreas, and then passes through the small intestine, where digestion continues.
The parietal cells in the fundus of the stomach, produce intrinsic factor, a glycoprotein which is essential for the absorption of vitamin B12.
Vitamin B12 is carried to, and through the stomach, bound to a glycoprotein secreted by the salivary glands – transcobalamin I .
Transcobalamin I protects the acid-sensitive vitamin from the acidic stomach contents.
In the more neutral duodenum, pancreatic enzymes break down the protective glycoprotein, freeing vitamin B12 which then binds to intrinsic factor which is then able to be absorbed by the enterocytes in the ileum.
The stomach is a distensible organ.
The stomach can normally expand to hold about one liter of food.
Its ability to expand i due to a series of gastric folds in the inner walls of the stomach.
The stomach of a newborn baby is only be able to expand to retain about 30 ml.
The spleen is the largest lymphoid organ in the body, and breaks down both red and white blood cells that are spent.
A product of this digestion of RBCs is the pigment bilirubin, which is sent to the liver and secreted in the bile.
Another product is iron, which is returned to the bone marrow to be used in the formation of new blood cells.
The second largest organ, after the skin, the liver is an accessory digestive gland which plays a role in the body’s metabolism.
The liver detoxifies various metabolites; synthesizes proteins and produce biochemicals needed for digestion.
The liver It regulates the storage of glycogen which it can form from glucose.
The liver can synthesise glucose from certain amino acids.
The liver’s digestive functions are involved with the breaking down of carbohydrates, and maintains protein metabolism in its synthesis and degradation.
It synthesizes cholesterol, and the bulk of lipoproteins.
Fats are also produced in the process of lipogenesis.
The liver sits on the right side of the abdomen, below the diaphragm, to the right of the stomach and it overlies the gall bladder.
The liver synthesises bile acids and lecithin to promote the digestion of fat.
Bile is produced by the liver and is made up of water (97%), bile salts, mucus and pigments, 1% fats and inorganic salts.
Bilirubin is its major pigment.
Bile acts partly as a surfactant lowering the surface tension between either two liquids or a solid and a liquid and helps to emulsify the fats in the chyme.
Food fat is dispersed by the action of bile into smaller units called micelles.
Micelles creates a much larger surface area for the pancreatic enzyme, lipase to work on.
Lipase digests the triglycerides which are broken down into two fatty acids and a monoglyceride.
These are then absorbed by villi on the small intestinal wall.
Bile also helps in the absorption of vitamin K from the diet.
Bile is collected and delivered through the common hepatic duct.
The common hepatic duct joins with the cystic duct to connect in a common bile duct with the gallbladder.
Bile is stored in the gallbladder for release when food is discharged into the duodenum.
The gallbladder is a hollow part of the biliary tract that sits just beneath the liver, with the gallbladder body resting in a small depression.
Bile produced by the liver is stored, before being released into the small intestine.
Bile flows from the liver through the bile ducts and into the gall bladder for storage.
Bile is released in response to cholecystokinin (CCK) a peptide hormone released from the duodenum.
CCK is produced by endocrine cells of the duodenum, and is stimulated by the presence of fat in the duodenum.
The gallbladder divided into three sections, a fundus, body and neck.
The neck gallbladder neck tapers and connects to the biliary tract via the cystic duct, which then joins the common hepatic duct to form the common bile duct.
It is at this junction is a mucosal fold called Hartmann’s pouch, where gallstones commonly get stuck.
The muscular layer of the body of the gallbladder contracts, so that it can discharge its bile into the bile duct.
The gallbladder stores bile in a natural, semi-liquid form at all times.
There are hydrogen ions secreted from the inner lining of the gallbladder that keep the bile acidic enough to prevent bile hardening.
Water and electrolytes from the digestion system are added to dilute the bile.
Salts attach themselves to cholesterol molecules in the bile to keep them from crystallizing.
If there is excess cholesterol or bilirubin in the bile, or if the gallbladder does not empty properly the systems can fail.
Gallstones form when calcium gets coated with either cholesterol or bilirubin and the bile crystallizes and forms a gallstone.
The gallbladder stores and releases bile into the small intestine in and helps in the digestion of fats by breaking down larger molecules into smaller ones.
Bile is also absorbed and transported back to the liver for reuse.
The pancreas is functioning as an accessory digestive gland, and is both an endocrine gland and an exocrine gland.
The endocrine part secretes insulin, which moves glucose from the blood into the muscles and other tissues for use as energy.
The endocrine part releases glucagon when the blood sugar is low; glucagon allows stored sugar to be broken down into glucose by the liver in order to re-balance the sugar levels.
The pancreas produces and releases digestive enzymes in the pancreatic juice that it delivers to the duodenum.
The pancreas connects to the duodenum via the pancreatic duct which it joins near to the bile duct’s connection where both the bile and pancreatic juice can act on the chyme that is released from the stomach into the duodenum.
Aqueous pancreatic secretions from pancreatic duct cells contain bicarbonate ions which are alkaline and help with the bile to neutralize the acidic chyme that is churned out by the stomach.
The pancreas is also the main source of enzymes for the digestion of fats and proteins.
Some of these are released in response to the production of CKK in the duodenum.
The cells are filled with secretory granules containing the precursor digestive enzymes.
The major proteases, the pancreatic enzymes which work on proteins, are trypsinogen and chymotrypsinogen.
Elastase is also produced.
Smaller amounts of lipase and amylase, phospholipase A2, lysophospholipase, and cholesterol esterase are secreted.
Zzymogens, are inactive variants of the enzymes; which avoids the onset of pancreatitis caused by autodegradation.
Once released in the small intestine the enzyme enteropeptidase activates trypsinogen by cleaving it to form trypsin; further cleavage results in chymotrypsin.
The lower gastrointestinal tract (GI), includes the small intestine and all of the large intestine.
The lower GI starts at the pyloric sphincter of the stomach and finishes at the anus.
The small intestine is subdivided into the duodenum, the jejunum and the ileum.
The cecum marks the division between the small and large intestine.
The large intestine includes the rectum and anal canal.
Partially digested food starts to arrive in the small intestine as semi-liquid chyme, one hour after it is eaten.
The stomach is half empty after an average of 1.2 hours.
After four or five hours the stomach has emptied.
The pH is crucial Inthe small intestine to activate enzymes
The chyme is very acidic, with a low pH, having been released from the stomach and needs to be made much more alkaline.
Small bowel alkalinity is achieved in the duodenum by the addition of bile from the gall bladder combined with the bicarbonate secretions from the pancreatic duct and also from secretions of bicarbonate-rich mucus from duodenal glands known as Brunner’s glands.
The resulting alkaline fluid mix neutralizes the gastric acid chyme which would damage the lining of the intestine.
The mucus component lubricates the walls of the intestine.
Food is digested food and reduced enough in size and composition to be absorbed by the intestinal wall and carried to the bloodstream.
Chyme is delivered to the duodenal bulb, and passes into the first of the three sections of the small intestine, the duodenum, jejunum and the the ileum.
The duodenum is the first and shortest section of the small intestine.
The duodenum is a hollow, jointed C-shaped tube connecting the stomach to the jejunum.
The duodenum starts at the duodenal bulb and ends at the suspensory muscle of duodenum.
The suspensory muscle to the diaphragm helps the passage of food by making a wider angle at its attachment.
Most food digestion occurs in the small intestine.
Segmentation contractions mix and move the chyme slowly in the small intestine allowing more time for absorption.
In the duodenum, pancreatic lipase is secreted to further digest the fat content of the chyme.
As a result smaller particles of emulsified fats called chylomicrons are produced.
Digestive cells, enterocytes, line the intestines, the majority being in the small intestine.
Enterocytes have villi on their surface which in turn have innumerable microvilli on their surface.
Villi create a greater surface area, not only for the absorption of chyme but for digestion by large numbers of digestive enzymes present on the microvilli.
Chylomicrons are small enough to pass through the enterocyte villi and enter into their lymph capillaries called lacteals.
Chyle is a milky fluid consisting mainly of the emulsified fats of the chylomicrons, that results from the absorbed mix with the lymph in the lacteals.
Chyle is then transported through the lymphatic system to the rest of the body.
The suspensory muscle marks
At the end of the duodenum, the suspensory muscle marks and the division between the upper gastrointestinal tract and the lower GI tract.
The digestive tract continues as the jejunum which continues as the ileum.
The jejunum, is the midsection of the small intestine.
The jejunum contains circular folds, flaps of doubled mucosal membrane which partially encircle and sometimes completely encircle the lumen of the intestine.
These circular folds together with villi serve increasing the surface area of the jejunum enabling an increased absorption of digested sugars, amino acids and fatty acids into the bloodstream.
The circular folds slow the passage of food so more time for nutrients are available to be absorbed.
The last part of the small intestine, the ileum contains villi: vitamin B12 and bile acids and any residue nutrients are absorbed here.
When the chyme is relieved of its nutrients the remaining waste material changes into feces, which pass to the large intestine, where bacteria in the gut flora further break down residual proteins and starches.
The transit time through the small intestine is an average of 4 hours.
Half of the food residues of a meal have emptied from the small intestine by an average of 5.4 hours after ingestion.
Emptying of the small intestine is complete after an average of 8.6 hours.
The cecum marks the division between the small intestine and the large intestine, and lies below the ileocecal valve in the lower right quadrant of the abdomen.
The cecum receives chyme from the small intestine, the ileum, and connects to the ascending colon of the large intestine.
The junction of the small intestine and cecum has a sphincter or valve.
The ileocecal valve slows the passage of chyme from the ileum, allowing further digestion.
The ileocecal valve is also the site of the appendix attachment.
In the large intestine, the passage of the digesting food in the colon is a lot slower, than in the small evaluation, taking from 30 to 40 hours until it is removed by defecation.
The colon is a site for the fermentation of digestible matter by the gut flora.
Feces are removed by the coordinated contractions of the intestinal walls, (peristalsis)m, which propels the excreta forward to reach the rectum and exit through the anus via defecation.
The wall of the colon has an outer layer of longitudinal muscles, the taeniae coli, and an inner layer of circular muscles.
The circular muscle keeps the stool moving forward and also prevents any back flow of waste.
The taeniae coli are responsible for the haustra bulges present in the colon.
Most parts of the GI tract are covered with serous membranes and have a mesentery.
Other more muscular parts of the GI tract lined with adventitia.
The celiac artery is the first major branch from the abdominal aorta, and is the only major artery that nourishes the gastrointestinal organs.
The celiac artery has three main divisions – the left gastric artery, the common hepatic artery and the splenic artery.
It supplies the liver, stomach, spleen and the upper 1/3 of the duodenum to the sphincter of Oddi, and the pancreas with blood.
Most of the blood is returned to the liver via the portal venous system for detoxification before returning to the systemic circulation via the hepatic veins.
The next branch of the abdominal aorta is the superior mesenteric artery, supplying the regions of the digestive tract derived from the midgut, which includes the distal 2/3 of the duodenum, jejunum, ileum, cecum, appendix, ascending colon, and the proximal 2/3 of the transverse colon.
The final branch for the digestive system is the inferior mesenteric artery, which supplies the regions of the digestive tract derived from the hindgut, which includes the distal 1/3 of the transverse colon, descending colon, sigmoid colon, rectum, and the anus above the pectinate line.
Blood flow to the digestive tract reaches its maximum 20–40 minutes after a meal and lasts for 1.5–2 hours.
The enteric nervous system consists of some one hundred million neurons embedded in the peritoneum, and the lining of the gastrointestinal tract extending from the esophagus to the anus.
These enteric neurons are collected into two plexuses – the myenteric (or Auerbach’s) plexus that lies between the longitudinal and the smooth muscle layers, and the submucosal (or Meissner’s) plexus that lies between the circular smooth muscle layer and the mucosa.
The parasympathetic innervation to the ascending colon is supplied by the vagus nerve.
Most of the digestive tract is innervated by the two large celiac ganglia, with the upper part of each ganglion joined by the greater splanchnic nerve and the lower parts joined by the lesser splanchnic nerve.

 See Gasrointestinal tract
See Gasrointestinal tract