 High flow nasal cannula therapy, also known as Heated humidified high-flow (HHHF) therapy, often also high flow nasal cannula(e) (HFNC) or high flow nasal oxygen (HFNO), is a type of respiratory support method that delivers a high flow oxygen through a nasal cannula intended to create a wash-out of the upper airway.
High flow nasal cannula therapy, also known as Heated humidified high-flow (HHHF) therapy, often also high flow nasal cannula(e) (HFNC) or high flow nasal oxygen (HFNO), is a type of respiratory support method that delivers a high flow oxygen through a nasal cannula intended to create a wash-out of the upper airway.
High-Flow Nasal Cannula with
High gas flow rates (≥30 liters per minute and up to 60 to 80 liters per minute) with a set fraction of inspired oxygen (Fio2) of 0.21 to 1.0 can be administered through a nasal cannula.
The applied gas is heated to match human body temperature (37 °C) and humidified targeting the body’s saturation vapor pressure. Heating (to 34° to 37°C) and humidification make gas delivery comfortable, and the high flow, usually higher than the patient’s own inspiratory peak flow, allows for the effective delivery of the intended Fio2.
High flows generate a small level of nonadjustable PEEP — slightly higher when the mouth is kept closed — and reduce ventilation requirements and inspiratory muscle effort through a washout of the dead space in the upper airway during expiration.
It is used in acute and chronic breathing problems.
It is useful in patients that are spontaneously breathing but have an increased work of breathing:
general respiratory failure, asthma exacerbation, COPD exacerbation, bronchiolitis, pneumonia, and congestive heart failure.
HHHF therapy has been used with general anaesthesia to facilitate surgery for airway obstruction.
HHHF therapy is useful in neonatal intensive care settings for premature infants with Infant respiratory distress syndrome.
HHHF therapy prevents in many infants the need for artificial ventilation via intubation, and allows safe respiratory management at lower FiO2 levels, and thus reduces the risk of retinopathy of prematurity and oxygen toxicity.
The cannula improves respiratory distress, oxygen saturation, and patient’s comfort.
HH mechanism of action is the application of mild positive airway pressure and lung volume recruitment.
It delivers higher FiO2 to the patient than is possible with typical oxygen delivery therapy without the use of a non-rebreather mask or tracheal intubation.
The heated humidification of the respiratory gas facilitates secretion clearance and decreases the development of bronchial hyper-response symptoms.
Some patients requiring respiratory support for bronchospasm benefit using air delivered by HHFT without additional oxygen.
HHFT is useful in the treatment of sleep apnea.
During use of HHHFT the patient can speak.
It is a non-invasive therapy that avoids the risk of ventilator-associated pneumonia in situations where it can supplant the use of a ventilator.
The use of nasal high flow in acute hypoxemic respiratory failure does not affect mortality or length of stay either in hospital or in the intensive care unit.
HHHFT does reduce the need for tracheal intubation by 15% and escalation of oxygenation and respiratory support, patients feel more comfortable, less breathless, and there is little evidence of harm.
Oxygenation is achieved by providing an increased FiO2 in the air flow.
A small diameter delivery system with a small-bore nasal cannula allows the flow that would traditionally move slowly through the upper airway to move quickly and maintain a constant stream of fresh gas which effectively washes out upper airway dead space.
The constant stream of fresh gas flow assists exhalation effort by flushing the exhaled air out to maintain this reservoir of fresh air ready to be inhaled.
The higher the flow, the more important proper humidification of the flow becomes.
Without humidity, the oxygenation and ventilation effects of high-flow therapy would be negated by the impact that dry air has on lung tissue.
Nasal cannula gas delivery is usually limited to delivery of 1–6 liters of flow per minute.
The percent oxygen inhaled by the patient (FiO2), usually ranges roughly 24–35% as the pure oxygen delivered from the cannula is diluted by entrainment of ambient air (21% oxygen).
Delivering oxygen using typical nasal cannula are limited because medical oxygen is anhydrous.
As the oxygen delivered from a pressurized source cools, the gas expands with the drop in atmospheric pressure.
The delivery of cold dry gas is irritating to the respiratory mucosa, causes drying and bleeding of the nasal mucosa and can increase metabolic demand by cooling the body.
The inspiratory flow rate at the nares of an adult usually exceeds 12 liters per minute, and can exceed 30 liters a minute for someone with mild respiratory distress.
Traditional oxygen therapy is limited to six liters per minute, does not begin to approach the inspiratory demand of an adult, and therefore the oxygen is diluted with room air during inspiration.
Prior to the advent of HFT, when increased FiO2 was required for respiratory support; special face masks or intubation was required.
With High Flow Therapy, it is possible to deliver a respiratory gas flow volume sufficient to meet or exceed the patient’s inspiratory flow rate.
The gas is heated and humidified to condition the gas as increased flows would be detrimental to tissue if left dry and cool.
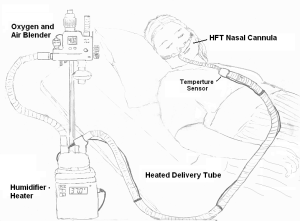
HFT oxygen is usually blended with compressed air.
Compressed oxygen and air are available for therapeutic use, allowing the delivery of air or blends of air and oxygen with the use of an oxygen blender.
The gas is heated, generally to about 37 °C, and humidified to near 100% RH using a humidifier.
The gas is transported through a heated delivery tube to prevent cooling and condensation of the water vapor that has been added to the respiratory gas.
HFT requires the use of nasal cannulae to deliver high flow rates and the pressure generated to do so.
The nasal cannula must be small enough not occlude more than 50% of the nares, allowing flow to have multiple points of exit for a continuous airway flush effect.
Among patient with respiratory failure due to Covid-19 high flow nasal cannula oxygen, compared with standard oxygen therapy, did not significantly reduce mortality.
Early use of nasal high flow oxygen therapy in children age 1 to 4 years with acute hypoxic, respiratory failure did not reduce the length of hospital stay compared with standard oxygen therapy (Franklin D).
