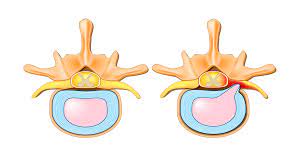
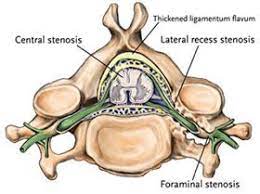
Foraminal stenosis is a medical condition that involves the narrowing of the spaces within the spine called the neural foramina.
These are small openings through which the nerve roots exit the spinal canal and travel to other parts of the body.
When these spaces become narrowed or obstructed, it can cause compression or pinching of the nerve roots.
This compression can lead to various symptoms, including:
Pain: Foraminal stenosis often causes localized pain in the neck or back, which can radiate down the arms or legs, depending on the location of the stenosis.
Numbness or tingling: Compression of the nerve roots can also lead to numbness or tingling sensations in the extremities.
Weakness: In some cases, muscle weakness or difficulty with coordination may occur due to the compromised nerve function.
The most common cause of foraminal stenosis is the gradual wear and tear of the spinal structures, known as degenerative changes.
These changes can include herniated discs, thickened ligaments, bone spurs, or inflammation, all of which contribute to narrowing the neural foramina.
Treatment for foraminal stenosis can vary depending on the severity of the symptoms and the underlying cause.
Non-surgical options may include physical therapy, pain management techniques, anti-inflammatory medications, and corticosteroid injections.
In more severe cases, surgical intervention such as a decompression surgery or a spinal fusion may be necessary to alleviate pressure on the nerve roots.
Foraminal stenosis is an important cause of radicular and generalized back pain.
Lateral root entrapment has an incidence of 8 to 11%.
In patients who do not respond to conservative interventions endoscopic spinal surgery provides similar results to open surgical approaches.
It may be the cause of pain in up to 60% of patients who remain symptomatic postoperatively.
Initial treatment for symptomatic foraminal stenosis is conservative methods:including mobilization, activity modification, anti-inflammatory medications, steroid injections, and selective nerve root block.
Patients refractory to conservative management are candidates for surgical decompression.
Open surgical approaches are associated with good outcome, a significant number of patients have postsurgical symptoms, including pain, weakness, and changes in sensorium.
An anterior surgical approach places the patient at risk of damage to important neurovascular structures, and both anterior and posterior approaches are associated with an increased risk of infection and neurological damage.
The procedure startss with intravenous antibiotics administered perioperatively, performed under anesthetic conscious sedation to aid in the protection of the nerves during the procedure.
The entry site is made with a stab wound through which a guide-wire is inserted down to the facet region of the vertebral body associated with stenosis.
A drill bit is used to create a window into the foraminal canal utilizing fluoroscopy.
Electrocautery and lasers are used for hemocoagulation and soft tissue removal.
Foraminal stenosis causing spinal nerve root compression that is amenable to both conservative and surgical treatments.
Open surgical decompression may be carried out via a midline approach, performing an interlaminar laminotomy, laminectomy, medial facetectomy, medial foraminotomy, or muscle-splitting or lateral approach with foraminotomy.
Cases requiring complete foraminal decompression may be treated with a combined interlaminar and lateral approach
Open surgical correction can be associated with blood loss, infection, prolonged hospital stay, and postoperative pain.
Endoscopic approaches, allow for shorter operating time, reduced exposure and manipulation and risk of damage of tissue, decreased length of hospital stay, and decrease in analgesics.
Endoscopic surgical treatment for foraminal stenosis is validated as a potentially effective alternative to open decompression.
Initial treatment for symptomatic foraminal stenosis includes mobilization, activity modification, anti-inflammatory medications, steroid injections, and selective nerve root block.
Patients refractory to conservative management are candidates for surgical decompression.
Anterior or posterior open surgical approaches are associated with good outcome, but many patients have postsurgical symptoms, including pain and weakness, and other risks.
Anterior and posterior surgery risk damage to neurovascular structures.
Endoscopic spinal surgery provides similar results to open surgical approaches with lower rates of complication, postoperative pain, and shorter duration of hospital stay.
Endoscopic surgical techniques are associated with a lower risk of infection and major neurovascular or organ damage, increased rate of recovery, and shorter duration of hospital stay.
The entry site is determined via fluoroscopy.
A scalpel is used to make a stab wound through which a guide-wire is inserted down to the facet region of the vertebral body associated with stenosis.
Over this guide-wire, a dilating system is used to dilate the tissues to approximately 14mm and a 12mm drill bit is used to create a window into the foraminal canal.
Foraminal stenosis causes spinal nerve root compression that is amenable to both conservative and surgical treatments.
Open surgical decompression may be carried out by a midline approach, which may be performed as interlaminar exposure, laminotomy, laminectomy, medial facetectomy, medial foraminotomy, or muscle-splitting or lateral approach with foraminotomy.
Treatment may require complete foraminal decompression with a combined interlaminar and lateral approach.
Laminectomy and foraminotomy are the most common open surgical treatment followed by laminotomy and foraminotomy, with good results reported in the majority of cases.
Open surgical correction is the current standard of care,
Surgical complications include: Blood loss, infection, prolonged hospital stay, and postoperative pain.
Endoscopic surgery allows for shorter operating time, reduction in tissue exposure and manipulation, and decreased risk of damage to surrounding structures, decreased hospital stay, decreased postoperative pain.
Trials evaluating endoscopic approaches for foraminal stenosis report positive results in 44-97% of cases.
