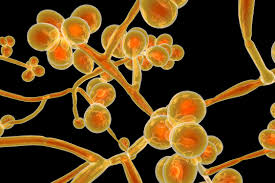
 Candida auris is a species of fungus that grows as yeast.
Candida auris is a species of fungus that grows as yeast.
It is one of the few species of the genus Candida which cause candidiasis in humans.
Often, candidiasis is acquired in hospitals by patients with weakened immune systems.
C. auris can cause invasive candidiasis, fungemia, in which the bloodstream, the central nervous system, and internal organs are infected.
It is easily misidentified as other Candida species.
It can remain viable for at least two weeks on plastic surfaces and for months on the skin.
It is more likely to resist antifungal agents, then other candida species.
Its spread within healthcare facilities and from one facility to another.
Most outbreaks of C. auris cases occur in high acuity post-acute care facilities.
It can easily travel from patient to patient or from a contaminated surface, such as a door knob to a patient.
As many is 90 to 95% of patients colonized with C auris are asymptomatic, but can spread the yeast to others.
Risk factors for colonization and infection are similar to those for candida species: advanced stage, diabetes, recent surgery, indwelling medical devices, immunosuppression, food, and stage kidney disease on dialysis, and received a broad-spectrum antimicrobials, including antifungals.
Hospitalizations within the prior year is a risk factor.
C. auris clinical presentation ranges from asymptomatic colonization to severe infections.
Colonization occurs on the skin, urinary, gastrointestinal and respiratory tracts prior to the development of infection.
The most common severe presentation of the infection is a fungemia, that may be related to the presence of an intravascular catheter.
The mortality rate for C auris candidiasis systemic aainfection involving the blood, brain, and heart or other parts of the body is thought to be as high as 60%.
C auris can survive in water and saltier environments, then other fungal pathogens.
Studies suggest 5 to 10% of patients colonized with C auris go on to develop an invasive infection.
It has multiple drug resistance.
More than 90% of C. auris isolates are resistant to fluconazole, and a range of 3–73% of C. auris isolates are resistant to voriconazole, while other triazoles of posaconazole, itraconazole, and isavuconazole have better activity.
Of C. auris isolates, 13% to 35% were reported resistant to amphotericin B.
30–60% of people with C. auris fungemia die.
There is currently no vaccine for Candida auris.
The C. auris genome encodes several genes for the ABC transporter family, a major facilitator superfamily associated with multiple drug resistance.
Its genome also encodes virulence-related gene families such as lipases, oligopeptide transporters, mannosyl transferases, biofilm formation, and transcription factors which facilitate colonization, invasion, and iron acquisition.
C. auris has distinct genotypes exist in different geographical regions with substantial genomic diversity.
Global warming will lead to selection of fungal lineages that are more thermally tolerant.
Diagnosis is difficult because it is phenotypically similar to other yeast species and frequently misidentified by testing.
Detection requires mass spectroscopy, or molecular identification, based on genetic sequencing.
Screening with axillary and groin swabs for culture or polymerase chain reaction testing is proposed for preventing outbreaks.
Treatment is complicated by resistance to anti-fungal agents.
Flucanazole resistance rates of 86 to 100% have been reported.
43% of isolates are resistant to amphotericin B.
Echinocandins resistance is the least prevalent occurring in 2 to 5% of isolates,and or the first line antimicrobials for invasive C auris infections.
Mortality associated with C auris fungemia ranges from 30 to 72%.
