 Tumor of unregulated astrocyte growth accounting for 25-30% of all gliomas.
Tumor of unregulated astrocyte growth accounting for 25-30% of all gliomas.
Falls into the largest category of tumors of intraepithelial tissue.
Characterized by prominent glial fibrillary acidic protein processes, typically also have mutations in IDH, but have intact 1p and 19q chromosomes as well as loss of ATRX.
Most astrocytomas display a loss of function mutations in tumor proteins, 53 (TP 53), and an alpha thalassemia/mental retardation, sex linked (ATRX), which is responsible for an abnormal telomere maintenance mechanism, known as alternative lengthening of telomeres.
Astrocytomas carry, IDH mutations with IDH 1 mutation R132H accounting for 90% of all IDH mutations and can be detected by immunohistochemistry.
Non-canonical IDH mutations, and IDH2 mutations are present in the remaining 10% of astrocytomas.
Do not metastasize through lymphatic or vascular systems.
Account for 80% of all gliomas and are the most common supratentorial tumors in all age groups.
Astrocytomas are primary intracranial tumors that develop from astrocytes.
These tumors may occur in many parts of the brain and/or spinal cord.
Astrocytomas are divided into two categories: low grade (I and II) and high grade (III and IV).
Low grade astrocytomas tumors are more common in children, and high grade tumors are more common in adults.
Malignant astrocytomas are more prevalent among men, contributing to worse survival.
WHO grade I pilocytic astrocytoma
WHO grade II astrocytoma-Diffuse astrocytoma
Fibrillary astrocytomas
Fibrillary astrocytomas are grade II tumors.
They grow relatively slowly so are usually considered benign, but they infiltrate the surrounding healthy tissue and can become malignant.
Fibrillary astrocytomas commonly occur in younger people, who often present with seizures.
Protoplasmic astrocytoma
Gemistocytic astrocytoma
WHO grade III astrocytoma-Anaplastic astrocytomas
WHO grade IV astrocytoma-Glioblastoma
Grade I and grade II referred to as low grade gliomas
Grade III and grade IV gliomas referred to as high-grade gliomas.
Giant cell Glioblastoma
Gliosarcoma
WHO grade II astrocytoma-Pleomorphic xanthoastrocytoma
Diffuse astrocytomas have hypercellularity, nuclear atypia, prominent mitotic activity and diffuse infiltration of surrounding brain tissue.
Diffuse astrocytomas have a tendency to have malignant transformation, and can change all the way to glioblastoma.
Diffuse astrocytomas include: protoplasmic, gemistocytic, fibrillary and mixed types.
Anaplastic astrocytoma, grade III astrocytoma by WHO classification.
Anaplastic astrocytoma has slow growth rate, moderate hypercellularity and moderate nuclear atypical and diffuse brain infiltration.
Anaplastic astrocytoma can result from the dedifferentiation of a grade II astrocytoma.
WHO grade II astrocytoma-Choroid glioma
WHO Pilocytic astrocytomas
WHO Subependymal giant-cell astrocytomas
Gliomatosis cerebri refers to an infiltrative malignancy involving 2 or more lobes of the brain.
Pilocytic astrocytomas and subependymal giant cell astrocytoma are of low or uncertain malignant potential.
Pilocytic astrocytomas frequently have BRAF alterations.
Pilocytic and subependymal astrocytomas are circumscribed lesions and do not invade surround tissues.
Pleomorphic xanthoastrocytoma are intermediate type lesions between circumscribed and invasive as they are circumscribed and slow growing, but malignant progression may occur.
In contrast to IDH-wild type glioblastoma it typically occurs in younger patients, often in the fourth and fifth decades of life.
First time seizures are the most common presentation, with less common manifestations, including headache, or focal neurological defects.
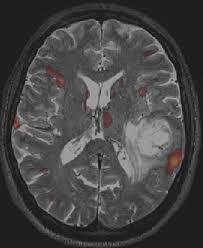
Contrast MRI is a standard assessment with a suspected glioma.
Astrocytoma Treatment & Management
Treatment options in astrocytomas include operative intervention and the use of chemotherapy and radiation therapy.
Adjuvant radiotherapy for pilocytic astrocytoma significantly prolonged progression-free survival (PFS) at both 5 years and 10 years compared with observation alone.
There is no accepted standard of treatment for low-grade or anaplastic astrocytoma.
Typically, anaplastic astrocytomas are treated with surgery, radiotherapy, and adjuvant temozolomide.
Some physicians add concomitant temozolomide, though no data from controlled trials exist to support concomitant temozolomide.
With anaplastic astrocytoma receiving adjuvant radiation, and concurrent treatment with temozolomide is associated with improved survival, as was isocitrate dehydrogenase (IDH) mutation.
Mproved 5-year survival is independently associated with concurrent temozolomide and IDH mutation.
Anaplastic astrocytomas are usually more responsive to chemotherapy than glioblastomas.
For recurrent anaplastic astrocytomas previously treated with nitrosoureas, temozolomide showed a 35% response rate, and provided an increased 6-month survival rate.
Treatment of low-grade astrocytomas is controversial as the role of surgical resection, timing of radiotherapy, and the role, timing, and appropriate agents of chemotherapy are not clear.
Controversy for treatment compounded by the relatively young age of the patients, the relatively indolent natural history of low-grade astrocytomas, and the morbidity associated with interventions.
Patients with a history of seizures should receive anticonvulsant therapy with monitoring of the drug concentration.
The use of anticonvulsants prophylactically in astrocytoma patients with no prior history of seizures remains controversial.
The use of corticosteroids, such as dexamethasone, yields rapid improvement in most patients secondary to a reduction of tumor mass effect.
Concurrent prophylaxis for gastrointestinal ulcers should be prescribed with corticosteroid administration.
Brainstem tumors account for 10-20% of all central nervous system tumors in the pediatric population.
Brainstem tumors are typically diagnosed in children 7-9 years old.
Brainstem gliomas typically depend on whether the tumor is diffuse or focal.
Diffuse brainstem gliomas make up 58-75% of all brainstem tumors, typically arise in the pons, and are noncircumscribed on MRI.
Diffuse brainstem gliomas are often malignant fibrillary astrocytomas (WHO grade III or IV) that infiltrate along white-matter tracts into the midbrain and thalamus and have a rapidly progressive and fatal course.
Diffuse brainstem gliomas clinically present with ataxia, cerebellar signs, and long tract signs.
When clinical and radiographic evidence suggests diffuse brainstem glioma, biopsy is of limited use as histology does not often alter treatment.
No treatment has been shown to cure or prolong survival in diffuse brainstem gliomas, including surgical resection.
Survival rates at 1-year survival has been shown to be 35-46%, and 3-year survival 11-17%.
Focal brainstem gliomas are usually WHO grade I or II, well-circumscribed on MRI with variable contrast enhancement, are more often found in the medulla and midbrain and have a much better prognosis than diffuse brainstem gliomas.
Surgery is often the primary treatment for focal brainstem gliomas as well as dorsal exophytic brainstem gliomas.
Obstructive hydrocephalus is common in astrocytomas, and is usually treated by either endoscopic third ventriculostomy or shunt placement.
In children with low-grade glioma, treatment with intensity-modulated radiotherapy (IMRT) after incomplete resection or disease progression provides local control rates comparable to those provided by 2-dimensional and 3-dimensional radiotherapy: The 8-year progression-free and overall survival rates with IMRT were 78.2% and 93.7%, respectively.
The roles of surgery with astrocytoma are: to remove or debulk the lesion, provide tissue for histological diagnosis, and assessment of prognosis, and allow a treatment plan.
Stereotactic biopsy is a safe and simple method for establishing a tissue diagnosis.
The use of stereotactic biopsy can be limited by sampling error and the risk of biopsy-induced intracerebral hemorrhage.
If hydrocephalus is present diversion of CSF by external ventricular drain (EVD) or ventriculoperitoneal shunt (VPS) may be required to decrease intracranial pressure as part of nonoperative management or prior to definitive surgical therapy.
Total resection of astrocytoma is often impossible because the tumors often invade into adjacent regions of the brain and exhibit tumor infiltration that is detectable only on a microscopic scale.
Surgical resection provides improved survival advantage and histological diagnosis, rather than offering a cure.
Complete resection of greater than 98% based on volumetric MRI, improves median survival compared with subtotal resection (13 vs 8.8 mo).
No specific drug treatment exists for low-grade glioma.
Certain conditions with low-grade astrocytoma typically require treatment: seizure prevention, and steroid therapy, usually combined with a gastroprotectant, is initiated for vasogenic edema around tumor.
It is postulated dexamethasone mechanisms of action in brain tumors include reduction in vascular permeability, cytotoxic effects on tumors, inhibition of tumor formation, and decreased CSF production.
Class Summary These agents inhibit cell growth and proliferation.
Temozolomide an oral alkylating agent converted is 100% bioavailable and approximately 35% crosses the blood-brain barrier.
While postoperative and postirradiation chemotherapy trials using nitrosourea and other agents are likely to benefit patients with malignant astrocytomas, the benefit for patients with well-differentiated astrocytomas is questionable.
Neurosurgery is generally intended to decrease tumor bulk while avoiding permanent neurological damage.
Prognosis for low-grade lesions after surgical intervention has been reported as 6-8 years.
For those patients who undergo surgical resection, the prognosis depends on whether the neoplasm evolves to a higher-grade lesion.
With anaplastic astrocytoma, symptomatic improvement or stabilization is the rule after surgical resection and irradiation.
60-80% of these patients have good quality and duration of survival, based on age, functional status, extent of resection, and adequacy of irradiation.
Irradiation of incompletely resected tumors can increase 5-year postoperative survival rates from 0-25% for low-grade astrocytomas and from 2-16% for anaplastic astrocytomas.
Patients with oligodendrogliomas that exhibit chromosomal changes at band 1p19q are known to have better responses to the procarbazine, lomustine (CCNU), vincristine (PCV) regimen of chemotherapy.
In high-grade astrocytoma, elevations in glioblastoma kallikrein 6 (KLK6), kallikrein 7 (KLK7), and kallikrein 9 (KLK9) proteins may have prognostic significance. utility as markers of patient survival.
