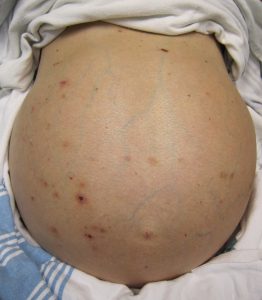
 Accumulation of fluid within the abdomen, peritoneal effusion.
Accumulation of fluid within the abdomen, peritoneal effusion.
Fluid in the peritoneal cavity is referred to as ascites and is due to increased hydrstatic pressure in the systemic circulation, increased peritoneal capillary permeability, decreased plasma oncotic pressure or decreased fluid reabsorption by lymphatics.
Most common cause in the US is cirrhosis, followed by malignancy, right sided heart failure, tuberculosis, pancreatic disease, rare infectious and hematologic diseases (Runyon BA).
10-15% of patients with gastrointestinal malignancies and 20% of patients with cancer of unknown primary develop ascites at some point in their disease.
Ovarian cancer makes up 20% of cancers with ascites.
Symptoms include nausea, pain, dyspnea, anorexia, early satiety, abdominal distension, and gastrointestinal dysfunction.
Evaluation of ascites includes estimate of jugular venous pressure helping to separate cardiac from noncardiac causes.
Paracentesis carries complication rate as high as 24%, including bowel perforation.
Paracentesis, The removal of fluid allows analysis of the fluid looking for white blood cell count, blood, cancer cells, and bacteria.
Peritoneal-venous shunts can be utilized but can cause infection, thrombophlebitis, bowel obstruction as well as dissemination of cancer cells in malignant ascites.
VEGF in very high concentration in malignant ascites and is responsible for increased vascular permeabilbity.
The reasons for ascites in patients with malignancy: spread to the peritoneum, and liver metastases causing increased pressure in the liver.
Analysis of fluid includes cell count, culture, albumin level, and cytology depending upon the clinical situation.
Chylous ascites may be caused by: obstruction of the lymph flow by external pressure resulting in leakage from dilated subserosal lymphatics into the peritoneal cavity, exudation of lymph via the walls of retroperitoneal vessels lacking valves into the peritoneal cavity , and from thoracic duct obstruction causing leakage of chyle.
Less commonly performed studies include triglycerides when looking for a chylous effusion, amylase when concerned about pancreatic disease, mycobacterial culture for tuberculous ascites and CEA for malignancy evaluation.
Serum-ascites albumin gradient (SAAG)-elevated levels> 1.1 g per dL associated with portal hypertension.
Serum-ascites albumin gradient (SAAG) is calculated by subtracting the value of ascitic fluid albumin from the value of serum albumin.
Cirrhosis, heart failure and Budd-Chiari syndrome associated with elevated SAAG.
Peritoneal metastases and tuberculosis associated with low SAAG.
SAAG is extremely helpful in determining the etiology of ascites.
SAAG may be superior to the total-protein- based exudate/transudate analysis.
SAAG often used to discriminate between liver disease and neoplastic etiology of ascites.
A low gradient (< 1.1 g/dL) indicates ascites of non-portal hypertensive etiology.
A SAAG value of 1.1 g/dL or greater is associated with portal hypertension with 97% accuracy as the cause of ascites.
A SAAG of less than 1.1 g/dL or his suggestive of other causes then portal hypertension and include: peritonealtuberculosis, the nephrotic syndrome, biliary ascites, peritoneal, bowel peroration, to infarction.
Only 13% of patients with malignancy associated ascites have a high SAAG without coexisting cirrhosis.
Peritoneal fluid that is bloody may be seen in trauma patients, and patients with ruptured spleen or liver, intestinal infarction, pancreatitis or malignancies.
Green colored ascites may result from the presence of bile such as may be seen in patients with perforated gall bladders, intestines or duodenal ulcers, cholecystitis, or acute pancreatitis.
More than several hundred milliliters of peritoneal fluid must accumulate before the diffusion can be detected by physical examination.
Large amount of ascitic fluid is associated with abdominal distention, abdominal discomfort, early satiety, anorexia, nausea, heartburn, pain, and respiratory distress.
Ultrasound and CT scan of the abdomen or sensitive diagnostic tests to indicate the presence of fluid.
Abdominal paracetensis with the removal of 50-100 cc is essential for establishing a differential diagnosis.
Paracentesis is a required procedure for patients with chronic ascites, ascites of unknown origin, sudden onset of ascites, suspected perforation of the gastrointestinal tract, and blunt trauma to the abdomen.
The two most common causes for ascites are complications of cirrhosiss and suspected intra-abdominal malignancy.
Laboratory assessment includes gross examination of the fluid for color and clarity, blood counts, differential leukocyte examination, analysis of total protein, amylase, LDH, microbial studies including Gram stain, routine cultures, anaerobic cultures, tuberculosis cultures, and cytologic examination.
Most commonly due to cirrhosis, severe liver disease or metastatic cancer, its presence can portend other significant medical problems.
Diagnosis of the cause is usually with blood tests, an ultrasound scan of the abdomen, and direct removal of the fluid by needle or paracentesis.
Patients complain of progressive abdominal heaviness and pressure as well as shortness of breath due to mechanical impingement on the diaphragm.
On physical examination ascites is apparent with abdominal bulging of the flanks in the reclining patient, difference in percussion noted in the flanks that shifts when the patient is turned, and the presence of a fluid wave/thrill.
Ascites exists in three grades:
Grade 1: mild, only visible on ultrasound and CT
Grade 2: detectable with flank bulging and shifting dullness
Grade 3: directly visible, confirmed with fluid thrill
Ultrasound investigation is often performed prior to paracentesis and may show the direction of flow in the portal vein, as well as detecting Budd-Chiari syndrome and portal vein thrombosis.
Causes of high SAAG (“transudate”) are:
Cirrhosis – 81% (alcoholic in 65%, viral in 10%, cryptogenic in 6%)
Heart failure – 3%
Hepatic Venous occlusion: Budd-Chiari syndrome or veno-occlusive disease
Constrictive pericarditis
Kwashiorkor (childhood protein-energy malnutrition)
Causes of low SAAG (“exudate”) are:
Nephrotic syndrome
Cancer (primary peritoneal carcinomatosis and metastasis) – 10%
Infection: Tuberculosis – 2% or Spontaneous bacterial peritonitis
Pancreatitis – 1%
Serositis
Hereditary angioedema
Other Rare causes:
Meigs syndrome
Vasculitis
Hypothyroidism
Renal Dialysis
Peritoneum Mesothelioma
Ascitic fluid can accumulate as a transudate or an exudate.
Amounts of up to 25 liters are possible.
Roughly, transudates are a result of increased pressure in the portal vein (>8 mmHg, usually around 20 mmHg[7]), e.g. due to cirrhosis, while exudates are actively secreted fluid due to inflammation or malignancy.
Exudate so are high in protein, high in lactate dehydrogenase, have a low pH (<7.30), a low glucose level, and more white blood cells.
Transudates have low protein (<30g/L), low LDH, high pH, normal glucose, and fewer than 1 white cell per 1000 mm³.
Clinically, the most useful measure is the difference between ascitic and serum albumin concentrations.
A difference of less than 1 g/dl (10 g/L) implies an exudate.
Portal hypertension plays an important role in the production of ascites by raising capillary hydrostatic pressure within the splanchnic bed.
Accumulation of fluid within the abdomen leads to additional fluid retention by the kidneys due to stimulatory effect on blood pressure hormones, notably aldosterone.
The sympathetic nervous system is also activated, and renin production is increased due to decreased perfusion of the kidney.
Extreme disruption of the renal blood flow can lead to hepatorenal syndrome.
Additional complications of ascites include spontaneous bacterial peritonitis (SBP), due to decreased antibacterial factors in the ascitic fluid such as complement.
Treated while an underlying etiology is sought, in order to prevent complications, relieve symptoms, and prevent further progression.
In patients with mild ascites, the goal is weight loss of no more than 1.0 kg/day for patients with both ascites and peripheral edema and no more than 0.5 kg/day for patients with ascites alone.
With severe ascites causing a tense abdomen, hospitalization is generally necessary for paracentesis.
Treatments in high SAAG, a transudate, are:
Salt restriction which allows diuresis, and is effective in about 15% of patients.
Since salt restriction is the basic concept in treatment, and aldosterone is one of the hormones that acts to increase salt retention,
A medication that counteracts aldosterone should be administered.
Spironolactone, or other distal-tubule diuretics triamterene or amiloride is the drug of choice since they block the aldosterone receptor in the collecting tubule.
Generally, the starting dose is oral spironolactone 100 mg/day (max 400 mg/day).
40% of patients will respond to spironolactone.
For nonresponders, a loop diuretic may also be added and generally, furosemide is added at a dose or alternatively bumetanide or Toresemide.
Monitoring diuresis by weighing daily.
The goal is weight loss of no more than 1.0 kg/day for patients with both ascites and peripheral edema and no more than 0.5 kg/day for patients with ascites alone.
If daily weights cannot be obtained, diuretics can also be guided by the urinary sodium concentration.
Dosage is increased until a negative sodium balance occurs, and a random urine sodium-to-potassium ratio of > 1 is 90% sensitivity in predicting negative balance (> 78-mmol/day sodium excretion).n
If a patient exhibits a resistance to or poor response to diuretic therapy, ultrafiltration may be needed to achieve adequate control of fluid retention and congestion.
Water restriction is needed if hyponatremia < 130 mmol per liter develops.
Main article: Paracentesis
With severe tense ascites, therapeutic paracentesis may be needed in addition to medical treatments listed above.
Albumin is generally administered intravenously in proportion to the amount of ascites removed.
Ascites that is refractory to medical therapy is an indication for liver transplantation.
With advanced cirrhosis that have recurrent ascites, shunts may be used such as portacaval shunt, peritoneovenous shunt, and the transjugular intrahepatic portosystemic shunt (TIPS).
None of these shunts has been shown to extend life expectancy, and are considered to be bridges to liver transplantation.
TIPS is more effective at removing ascites as compared with paracentesis,however, TIPS patients develop hepatic encephalopathy significantly more often.
Exudative ascites generally does not respond to manipulation of the salt balance or diuretic therapy.
Repeated paracentesis and treatment of the underlying cause is the mainstay of treatment.
Complications involve portal vein thrombosis and splenic vein thrombosis.
