 Tumors of the adrenal gland discovered incidentally during imaging studies done for purposes other than adrenal pathology.
Tumors of the adrenal gland discovered incidentally during imaging studies done for purposes other than adrenal pathology.
It is defined as a clinically unapparent adrenal lesion of 1 cm or greater in diameter detected on imaging performed for indications other than the evaluation of the adrenal disease.
Prevalence has increased dramatically in recent years due to the exponential growth in the use of CT and MRI imaging.
Found in 1-6% of abdominal imaging studies.
Uncommon under the age of 30 years, with a prevalence of 0.2%.
The prevalence is approximately 3% among patients in their 50s.
Prevalence is estimated to be approximately 3% at age 50 years and increases to 7-10% in 70-year-old patients.
Prevalence 7% in persons 70 years or older, and adrenal incidentaloma seen in up to 10% of the elderly (Kloos RT et al).
More than 80% of incidentalomas are benign.
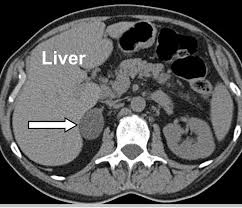
An adrenal adenoma is a benign tumor of the adrenal gland, located just above the kidney.
The analysis of patients in whom an adrenal incidentaloma is detected is to establish whether hormonal hypersecretion or malignancy is present.
In general, adrenal incidentaloma population has a little prevalence of clinically important pathology and is estimated that more than 70% of patients or eventually diagnosed as having benign, hormonally inactive adrenal adenoma.
Where adrenal mass is identified the key critical questions are: whether it functions, and whether it is malignant.
It is mandatory to rule out the presence of a pheochromocytoma, as if left untreated it could result in severe cardiovascular morbidity and mortality.
It is recommended to determine metanephrine levels in plasma or in a 24 hour urine collection in every patient with an adrenal incidentaloma.
Recent studies suggest that patients with a CT unenhanced attenuation value of 10 HU or less can exclude pheochromocytomas and metanephrine levels need not be investigated.
Some adrenal adenomas, are non-functioning adrenal adenomas, and do not secrete hormones, while others do.
Most adrenal adenomas have a high lipid contact content and enhanced a low density on CT.
Some adrenal adenomas secrete hormones that can cause different medical problems, depending on the type of hormone.
If an adrenal adenoma releases cortisol, the patient can develop Cushing’s Syndrome, also known as hypercorticism or hyperadrenocorticism.
Adrenal adenomas tend to have a genetic basis.
Adrenal metastases usually originated from primaries located in the lung, breast, melanoma, kidney, thyroid, and colon.
Usually only appear in adulthood..
About 6% of patients over 60 have an adrenal adenoma.
Most discovered through computed-tomography (CT) or magnetic-resonance imaging (MRI) scanning of the abdomen for unrelated reasons.
Adrenal adenomas are typically round, homogeneous, and relatively small.
Functioning adrenal adenomas can be treated through surgical removal of the adenoma, or adrenalectomy laparoscopy.
Eighty percent of adrenal adenomas are non-functioning, and do not cause any harm to the patient.
Most are nonfunctioning cortical adenomas with minimal or no clinical significance.
2.5% are metastatic disease to the adrenal glad from another cancer (Duh QY).
Meta-analysis of 32 studies 19% of adrenal incidentaloma lesions were metastases and 10% were primary adrenal cortical tumors (Mansmann G et al).
In metastatic adrenal lesions the median time to identification of adrenal metastases was 2.5 years from diagnosis of the primary cancer( Sagalowsky AL et a).
A large non-functioning adrenal tumor should be resected because of risk of malignancy.
Functional adrenal lesions secreting excess adrenal hormnes (cortisol, aldosterone, sex hormones, catecholamines) account for a significant number of cases, if left untreated may be associated with increased morbidity.
When an incidentalomas is not resected it should be monitored periodically for growth and hyperfunction.
Malignant lesions of the adrenal gland are rare.
In a retrospective review of 139 adrenal incidentalomas in Hong Kong, 43.9% were nonfunctional benign adrenal adenomas, 37.4% were functional lesions, and 10.8% were malignant lesions (Ng V et al).
In the above study 19.4% of functional lesions secreted excess cortisol, 8.6% secreted aldosterone, 8.6% secreted excess catecholamines and 0.7% had excess cortisol and aldosterone (Nf V et al).
