 Adrenal cancer is rare and accounts for 0.2% of all cancers.
Adrenal cancer is rare and accounts for 0.2% of all cancers.
Adrenal carcinomas are rare with an incidence of 0.7-2 cases per million inhabitants/year.
Adrenocortical carcinoma has an estimated prevalence of 4-12 per million population, in contrast to benign adrenocortical adenomas that occurred in at least 3% of the population over the age of 50 years.
Most common at middle-age to 40-60 years, and children younger than five years.
55 to 60% occur in females.
Rapidly growing malignant neoplasm with an estimated incidence of 1 to 2 per million people annually.
Prognosis is poor, and even with localized tumors metastases frequently develop within 6-24 months of surgical resection.
Over half of patients have stage III or stage IV at diagnosis, which has a poor prognosis.
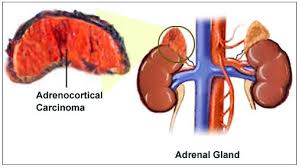
Tumors are typically 8 to 12 cm in diameter at the time of diagnosis, but approximately 40% do not present with clinically apparent hormone secretion.
Molecular clustering of subtypes are linked to outcomes, COC3 COC2, COC1 or associate with poor, intermediate, and better prognosis, respectively.
Complete surgical resection is only cure.
Local recurrence after surgical resection is estimated to be as high as 65%.
Patients with advanced disease such as a tumor greater than 8 cm, positive resection margins, incomplete resection, a high Ki-67 proliferation index of greater than 10%, rupture of the tumor capsule, or advanced stage at diagnosis are very high risk factors for locoregional recurrence.
Majority of cases are sporadic, although familial predisposition does occur.
Is often seen in individuals age 40 to 60 years old with a median age of 55 years at diagnosis.
Most cases are sporadic.
Is associated with the Li-Fraumeni syndrome, multiple endocrine neoplasia 1, Beckwith-Wiedemann syndrome, congenital adrenal hyperplasia, familial adenomatous polyposis, and Carney complex.
1-3% of adrenocortical cancers associated with Li-Fraumeni syndrome.
50-80% of pediatric patients have a germline TP53 mutation
Approximately 60% show clinical hormonal hypersecretion, and the remainder on non-functioning: acute hypercortisolism or hyperandrogenism.
Cushing’s syndrome, with or without virilization, as the most frequent presentation for a functioning adrenocortical carcinoma.
Cortisol secreting adrenocortical cancers have a poor overall prognosis, with a higher likelihood of metastases.
Has a bimodal age distribution wit peak incidences in early childhood and in the 4th-5th decades of life.
Female:male ratio of approximately 1.5 to 1.
60% adrenocortical carcinomas are functional, and 45% secrete both androgens and glucocorticoids, while the rest secrete glucocorticoids alone (45%), androgens alone (10%), or rarely, aldosterone (DeLellis RA).
Adrenal cortical tumors may be associated with hereditary cancers syndromes and inherited diseases and include: Carney complex, familial polyposis coli (FPC), Li-Fraumeni syndrome, Beckwih-Widemann, hereditary leimatosis, McCune-Albright syndrome, and MEN1.
European Network for the Study of Adrenal Tumors staging criteria
Stage I T1, N0, M0
Stage II T2, N0, M0
Stage III T1-T2, N1, M0 or T3-T4, N0-M1, M0
Stage IV T1-T4, N0-N1, M1
5 year survival rates using the above classification was 82% stage I, 61% stage II, 50% stage III, and 13% for stage IV.
Surgical resection is the primary treatment for patients with stage I to stage III disease.
The aim of surgery is to achieve a complete resection of the tumor, as prognosis is directly related to achieve clear margins.
With complete surgical resection five-year survival is 40-50%, and with incomplete resection median survival is less than one year.
Approximately 2/3 of patients with adrenocortical carcinoma may experience local regional recurrence after complete surgical resection.
Even after RO resection with negative margins, approximately 30% of patients may still experience a tumor recurrence, leading to a poor prognosis.
In patients who present with limited metastatic disease complete resection of primary and metastatic lesions provide benefit.
Adjuvant treatment has not proven to be beneficial in prolonging overall or disease free survival.
The role the role of adjuvant radiation therapy is debated, but some studies have suggested adjuvant radiation therapy with or without mototane therapy can lead to significant increase in local control.
Mitotane and cis-platinum based regimens associated with a 20% response rate in metastastic disease.
Thalidomide reported to be an active agent in metastases.
Using blood based next generation sequencing (ctDNA) to characterize genomics alterations in advanced disease is feasible in over 80% of patients.
