Adipose tissue, or fatty tissue is the body’s means of storing metabolic energy over extended periods of time.
Adipocytes store fat derived from the diet and from liver metabolism.
Adipose tissue is capable of more than doubling its mass and then returning to baseline.
Adipose tissue is an endocrine gland that releases hormones in the bioactive molecules referred to as adipokines.
Methods for assessing whole body adiposity include: computed tomography, MRI, dual energy x-ray absorptiometry, ultrasonography, and air displacement plethysmography.
Fat mass can be estimated rapidly who is the use of skinfold calipers, waist circumference, or BMI.
White adipose tissue officially stores sufficient energy to free humans from constantly seeking food, and permitting physical and mental efforts towards building civilization.
Fat is not one entity, but a collection of related but different anatomical and functional adipose tissue depots.
Adipose tissue releases immune modulators, such as cytokines and peptides that regulate blood pressure and clotting.
White adipose tissue regulates energy balance.
Brown adipose tissue consumes glucose and triglycerides, generating heat.
Brown adipose tissue is designed for non-shivering thermogenesis.
Brown fat in adults is limited to the neck, shoulders, posterior thorax, and abdomen, and these depots drain directly into the systemic circulation and may lead to more rapid distribution of warmed blood to the rest of the body.
White adipose tissue develops from mesoderm in the second trimester of pregnancy, and by birth there are both visceral and subcutaneous deposits.
White adipose tissue as a mesodermal organ communicates at the autocrine, paracrine, and endocrine levels.
Pregnancy requires a sufficient long-term supply of energy and white adipose tissue is essential for the proper function of the reproductive system, which includes the secretion of regulatory and sex hormones and lactation.
With too little white adipose tissue, is is seen in anorexia nervosa and lipodystrophies there is an interruption in menstruation.
Excessive white adipose tissue leads to early puberty.
White adipose tissue signals organs to coordinate the storage of consumption of nutrients within the liver and skeletal muscle.
Brown adipose tissue arises during the late second trimester and protects newborns from cold as they develop the ability to shiver.
In lean adults, the entire white adipose tissue depot ranges from 20 to 30 kg in women, or 30 to 40% of total body mass, and 10 to 20 kg in men and 15 to 25% of total body mass.
Many of the above factors, in addition to obesity, have been linked to increased risk of breast cancer, notably in postmenopausal women.
A major reservoir for adult stem cells with potential to develop into cardiomyocytes or endothelium.
Adipose tissue is a very active metabolic site that synthesizes and breaks down lipids and metabolized substrates, such as fatty acids and branched chain amino acids.
Adipose tissue dysfunction characterized by ectopic fat deposition in abdominal organs and liver, inflammatory and adipokine dysregulation and insulin resistance and may be an important mediator of the development of diabetes rather than total fat mass in obese individuals.
Adipose cells have pro-inflammatory activation, associated with insulin resistance.
Adipose tissue dysfunction decreases secretion of the insulin-sensitizing adipokine adiponectin in people with nonalcoholic fatty liver disease.
Adipose tissue secretes cytokines such as TNF, chemokines, hormones, and other inflammatory mediators, collectively called adipokines.
Adipose tissue also secretes the hormone leptin.
Considered as an endocrine organ that could play a role in tumor growth or differentiation by its secreted adipokines.
Adipokines can exert local biological effects and can circulate in the blood to cause distant organ changes.
Variation in body fat distribution, independent of generalized adiposity, is associated with differential metabolic risk factors.
The primary function of white adipose tissue is to store energy in the form of triglycerides.
Metabolic risks are do at least as much to the location of excess triglyceride storage as to the overall fat mass of the body.
White adipose tissues commonly separated into visceral fat and subcutaneous fat, confering negative and neutral or positive metabolic effects, respectively.
Visceral fat is divided into multiple distinct regions with different metabolic risks.
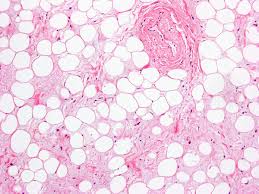
Adipose tissue is composed of multiple distinct types of cells including adipocytes, fibroblasts, blood and blood vessels, macrophages and other immune cells and nerve tissue.
Various proteins and proteoglycans in the extracellular matrix have active roles in the function of both white and brown adipose tissue.
The previous concept that humans are born with all their fat cells they will ever have, is incorrect.
Adipogenesis studies show that adipogenesis continues throughout life with the median turnover rate of 8% per year, indicating an entire replacement of the adipocytes in the body occurs every 15 years: similar to osteocytes and faster than the turnover of many cardiomyocytes.
Growth of adipocytes comes from hypertrophy and hyperplasia.
Among patients with known coronary artery disease, higher body fat percentage, but not BMI, is associated with a greater risk of major adverse cardiovascular events, suggesting the accuracy of BMI is not very good.
Fat stores stability is the result of intense negative feedback as the brain senses when stores are low and then promotes repletion by simultaneously decreasing energy expenditure and stimulating hunger.
Lower gluteofemoral or higher abdominal fat distribution are significantly associated with higher risk of coronary disease and type two diabetes.
The proportion of abdominal to gluteofemoral body fat correlates with obesity-associated diseases and mortality.
Population studies show that an increased gluteofemoral fat mass is independently associated with a protective lipid and glucose profile, as well as a decrease in cardiovascular and metabolic risk.
Studies of adipose tissue physiology confirm distinct properties of the gluteofemoral fat depot with regards to lipolysis and fatty acid uptake it appears to be more passive than the abdominal depot and it exerts its protective properties by long-term fatty acid storage.
Leptin and adiponectin levels are positively associated with gluteofemoral fat while the level of inflammatory cytokines is negatively associated.
Finally, loss of gluteofemoral fat, as observed in Cushing’s syndrome and lipodystrophy is associated with an increased metabolic and cardiovascular risk.
Gluteofemoral fat is a determinant of health by entrapment of excess fatty acids, thus protecting from the adverse effects associated with ectopic fat deposition.
Adipokines are expressed at much higher levels in the fat tissue of obese compared to lean individuals.
Macrophages accumulate in adipose tissue during the development obesity and are integral to the inflammatory state seen in obese and insulin resistant individuals.
Fat deposits include visceral adipose tissue, abdominal subcutaneous adipose tissue, lower body fat and liver fat.
Abdominal subcutaneous tissue, abdominal visceral adipose tissue, intramuscular fat, intrathoracic fat, pericardial sac, thoracic periaortic fat, intrahepatic fat, renal sinus fat, are all individually associated with more adverse cardiometabolic risk factors.
Visceral fat linked to elevated blood pressure values and greater prevalence of hypertension, independent of total body weight and subcutaneous adiposity.
Accumulation of visceral adipose tissue is associated with increased risk of cardiovascular disease, type two diabetes, and cancer.
Adipose tissue information is likely responsible for cardiovascular disorders and psoriasis including accelerated coronary atherosclerosis leading to myocardial infarction, atrial myopathy leading to atrial fibrillation and thromboembolic stroke, and ventricular myopathy leading to heart failure with a preserved ejection fraction.
Lower body fat is significantly and independently associated with lower cancer risk.
Reductions in bodyweight and visceral adipose tissue in particular, have the potential to substantially reduce the risk of cardio metabolic disease.
Adipose fat deposits such as visceral adipose tissue, abdominal subcutaneous tissue and liver fat are associated with different effects on metabolic and cardiovascular disease risk.
Adipose tissue stores lipids in the form of triglycerides, slowly releasing them into the bloodstream when insulin is low.
In insulin-resistant adipose tissue-obesity and type 2 diabetes-more triglycerides are broken down into FFAs and released into the bloodstream, promoting uptake by the liver.
White, and more recently brown adipose tissue have been identified as integral and regulateb lecomponents of lipoprotein and bile acid metabolism.
Triglyceride rich lipoproteins in the form of chylomicrons, and liver derived very low density lipoproteins deliver their lipid payloads to white and brown adipose tissues.
Postmenopausal women have changes in body fat distribution, primarily a greater tendency for central fat distribution compared with age and BMI matched premenopausal counterparts.
Age and BMI matched women, those who are postmenopausal tend to have a greater percentage of body fat in the central distribution as compared with premenopausal women.
Visceral fat deposits may increase 15 – 20% of the total body fat compared with 5 – 8% in the premenopausal state.
Abdominal visceral adipose tissue is a pathogenic fat depot associated with the metabolic syndrome.
Fat tissue location determines its metabolic profile: visceral fat is located within the abdominal wall, subcutaneous fat is located beneath the skin.
Visceral fat produce signaling chemicals/ hormones among which several are involved in inflammatory tissue responses.
One of these hormones is resistin which has been linked to obesity, insulin resistance, and Type 2 diabetes.
Metabolically obese normal weight appear to be healthy but have a higher risk of cardiometabolic disease, such as diabetes and coronary arteries ease, and possibly cancer.
Lower levels of gluteofemoral (hip) fat is associated with a higher levels of type two diabetes and coronary disease risk.
Upper body subcutaneous fat is a separate compartment from abdominal subcutaneous fat.
Higher upper body subcutaneous fat is associated with adverse cardiometabolic risk factors.
Both white and brown adipose tissue participate in immunomodulation, the suppression and activation of the immune system, and each tissue releases a profile of mediators of the complement system.
Obesity leads to white adipose tissue pro-inflammatory cytokines such as TNF-alpha, interleukin – 1 beta, interleukin 6 , and interferon-gamma: these factors activated recruit macrophages, which increase from less than 10% to nearly 40% of the total number of cells in adipose tissue.
CD4 and CD8 cells, dendritic cells, and B cells join in adipose tissue.
Adipocyte insulin resistance in macrophages activation is increased fatty acid release which drives synthetic gluconeogenesis and hyperglycemia.
Experimental studies have shown that upper body fat is the primary source of circulating free fatty acids and a strong determinant of insulin resistance (Martin MI).
Neck circumference can be used as an indirect measure of upper body subcutaneous fat, and is associated with cardio metabolic risk factors and subclinical atherosclerosis.
Diseases associated with predilection to accumulate upper body fat include: Cushing syndrome, lipodystrophy, HIV associated lipodystrophy-all of which have been linked to metabolic impairments.
