Rare process with a prevalence of 10 cases per million people.
Due to pituitary tumors arising in somatotroph cells with aberrant secretion of growth hormone.
High growth hormone and insulin-like growth factor 1 levels are associated with somatic and metabolic dysfunction.
Approximately 70% of patients with acromegaly have invasive macroadenoma at diagnosis.
It may be associated with germline AIP mutations, the McCune-Albright syndrome, or acidophilic stem cell adenomas.
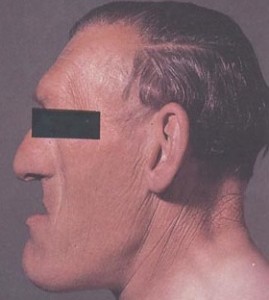
Clinical findings may include: frontal bossing, prognathism, deep nasolabial folds, thickened skull, widened spacing in teeth, facial edema, underbite, macroglossia, enlargement of feet, hands, excessive sweating, acne, headache, diabetes, thickened skin, skin tags, tall stature, insulin resistance, hypogonadism, hypertension, sleep apnea, arthralgia, carpal tunnel syndrome, colon polyps, and cardiac valve dysfunction.
Acromegaly is characterized by facial and cranial changes, such as frontal bossing, large nose and lips, increased dental spacing, and prognathism, and acral enlargement in 95%, headache in 60% of patients, arthropathy in 70% of patients, hyperhidrosis in 65% of patients and compressed or collapsed vertebrae in 50% of patients, diabetes, or pre-diabetes in 50% of patients, hypertension in 35%, cardiomyopathy leading to congestive heart failure in 10%, valvular heart disease up to 30%, sleep apnea 65%, carpal tunnel syndrome 64% and hyperprolactinemia 30%.
Coexisting conditions include headache and acral and soft tissue changes.
Slowly progressive enlargement of the face and extremities associated with cardiac, rheumatologic, restpiratory, and metabolic abnormalities tied to elevations in circulating growth hormone and insulin like growth factor-1.
Prognathism leads to incisor separation and jaw malocclusion.
Obstructive sleep apnea and excessive snoring are hallmarks of uncontrolled acromegaly.
Arthropathy is reported in about 70% of patients with polyarticular arthritis, osteophytosis, dorsal kyphosis, and vertebral fractures.
Associated with structural changes including: thickening of the heart muscle, dilatation of the ventricles, diminished diastolic function, hypertension, arrhythmias. left ventricular dysfunction, and an increase the aortic root diameter.
Structural changes are compounded by common comorbidities which include: hypertension, dyslipidemia, insulin resistance, and glucose intolerance with increased risk of diabetes.
About 30% of patients with acromegaly have high prolactin levels, often with galactorrhea.
Colon polyps were detected in 32% of patients.
Acromegaly is associated with increased incidence of cancer: colorectal, kidney, and thyroid: not confirmed in other studies.
Higher death rates associated with acromegaly due to cardiovascular, respiratory and cerebrovascular disorders and also possibly cancer.
Somatotroph cells originate in the anterior pituitary gland producing an excess of growth hormone.
Somatotroph cell development and proliferation related to the Prophet of Pit-1 (PROP1) gene which controls embryonic development of cells of the Pit-1 transcription factor lineage.
Growth hormone secreted as a 191 amino acid, 4-helix bundle protein and a less abundant 176 amino acid form which enter the circulation under the control of the hypothalamic releasing and hypothalamic inhibiting hormones that traverse the hypophysial portal system by influencing specific somatotrophic surface receptors.
Release of growth hormone is pulsatile in nature.
Growth hormone releasing hormone induces synthesis and secretion of the hormone while somatostatin suppresses its secretion.
Finding of elevated serum level of insulin like growth factor (IGF-1) is suggestive of acromegaly.
Diagnosis can be delayed by approximately 10 years after the onset of symptoms as patients first seek dental, orthopedic, rheumatologic, or cardiac care.
Approximately 20% of patients seekcare because of altered facial appearance, enlarge the extremities, or both.
Diagnosis confirmed by lack of growth hormone suppression after glucose suppression testing.
Binding of growth hormone to hepatic receptors leads to systemic release of IGF-1.
Growth hormone regulated by ghrelin.
Affects the entire body with risk of substantial morbidity and premature mortality if not recognized and treated.
Diagnosis delay averages 8-10 years, with alternative diagnoses of diabetes, hypertension, osteoarthritis, carpal tunnel syndrome, joint replacement, sleep apnea, malocclusion and renal stones being made before the appropriate diagnosis.
Hypertension results from sodium returning affects of growth hormone, inhibition in atrial natriuretic peptide by insulin like growth factor-1, and increased peripheral vascular resistance triggered by both hormones.
Excess growth hormone increases production of pro inflammatory mediators that degrade structural elements of the aortic and mitral valve, precipitating regurgitation .
Associated with progressive myocardial fibrosis and involvement of the conduction system of the heart increase the risk for arrhythmias and conduction disorders.
Altered hormonal activity changes In the sympathoadrenalmedullary pathway, promotes endothelial dysfunction, valvular disease and cardiomyopathy.
In normal persons growth hormone levels are usually undetectable through most of the day but there are approximately 10 intermittent pulses of growth hormone per 24 hour, most often at night when the level can be as high as 30 microgm per liter.
Peaks of growth hormones may overlap with elevated levels as seen in acromegaly.
Fasting increases secretion of growth hormone, while aging and obesity decrease bursts of the hormone.
Fasting or random growth hormone level results may be normal because of the pulsatile secretion of the hormone and the impracticality of measuring pulsatile levels.
Definitive testing for the diagnosis is the use of the oral glucose tolerance test and measurement of growth hormone every 30 minutes for 2 hours.
Best screening test measurement of serum insulin like growth factor 1 (IGF-1) level.
IGF-1 elevated levels for the patient’s age are highly specific for acromegaly and correlate with disease activity.
Because of the pulsatile nature of adenoma growth hormone secretion reliance on random measurement for diagnosis of IGF-1 is precluded.
IGF-1 an integrated measure of overall growth hormone secretion.
IGF-1 varies with age and decreases with age.
IGF-1 falsely elevated in pregnancy as placental production of a growth hormone variant that stimulates production of IGF-1.
Diagnosis of acromegaly is established by using an ultra sensitive assay to document nadir growth hormone levels of more than 0.4 µg per liter during a 75 g glucose load.
TREATMENT:
Treatment goals include ablating or controlling the pituitary mass, suppressing growth hormone and IGF-1 hypersecretion, and preventing the development of associated disorders while maintaining anterior pituitary function.
Medical therapy is generally reserved for those with persistent or recurrent disease after pituitary surgery.
Surgical resection resulted in control of growth hormone secretion and IGF-1 levels in 73% of patients with micro adenomas AND 61% of patients with macroadenomas.
In patients with macroadenoma invding the cavernous sinus show persistent growth hormone hypersecretion after surgery.
Radiosurgery shows biochemical remission it up to 59% of patients, with the meantime to remission of 38 months and the meantime to recurrence of 17 months.
Somatostatin receptor ligands octreotide and lanreotide inhibit growth hormone secretion and their usse is associated with an overall control of growth hormone secretion and of IGF-one levels in 55% of patients.
Somatostatin receptor ligands result in about a 53% reduction in tumor mass.
With the use of the agents, soft tissue swelling and headache usually resolve, sleep apnea abates, and left ventricular function improves, but hypertension may persist.
Dopamine agonist for a patient with mild disease may normalize IGF-one levels in some patients with disease that is resistant to somatostatin therapy.
Pegvisomant is a growth hormone receptor antagonist that blocks peripheral growth hormone action and subsequent IGF-1 production is useful for patients with resistant disease to somatostatin receptor ligands as well as in patients with hyperglycemia: the drug enhances insulin sensitivity.
Pegvisomant added to Pituitary directed somatostatin receptor ligand offers greater efficacy then either drug alone.
Pegvisomant and pasireotide are associated with high likelihood of effectivity in the most effective single agents.
In patients treated for acromegaly all cause mortality is not increased above the general population in patients who achieve a normal serum IGF –1 level.
