 Vulvodynia is a pain condition that affects the vulvar area and occurs without an identifiable cause.
Vulvodynia is a pain condition that affects the vulvar area and occurs without an identifiable cause.
Vulvodynia symptoms typically include a feeling of burning or irritation.
For the diagnosis to be made symptoms must last at least three months.
The causes of vulvodynia including an excess of nerve fibers, hormonal imbalances, inflammation, and muscular dysfunction.
Factors influencing vulvodynia may include genetics, immunology, and possibly diet.
Diagnosis is by exclusion other possible causes.
Diagnosis may or may not include a biopsy of the area.
Treatment: none is universally effective, and the evidence to support their effectiveness is often poor.
Measures include medications, pelvic floor physical therapy, surgery, and counselling.
Vulvodynia is estimated to affect up to 10-28% of women.
Pain is the most significant symptom of vulvodynia, and can be characterized as a burning, stinging, irritation or sharp occurring in the vulva and entrance to the vagina.
Pain may be constant, intermittent or happen only when the vulva is touched.
Vulvodynia usually has a long duration.
Symptoms may be localized or the entire vulvar area.
Symptoms can occur during or after sexual activity, when tampons are inserted, or when prolonged pressure is applied to the vulva, such as during sitting, bike riding, or horseback riding.
The pain can be provoked by touch or contabnt and unprovoked
Some cases of vulvodynia are idiopathic.
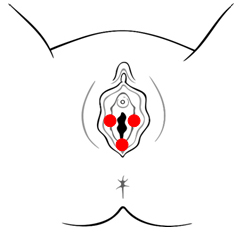
Vestibulodynia, refers to pain localized to the vestibular region.
It tends to be associated with a highly localized burning or “cutting type of pain.
Vestibulodynia is the most common subtype of vulvodynia that affects premenopausal women.
Vestibulodynia syndrome affects about 10%–15% of women seeking gynecological care.
The pain of vulvodynia may extend into the clitoris; clitorodynia.
Clitorodynia may be sometimes caused by clitoris adhesions.
Symptoms of clitodynia may include pain, hypersenstivity, hyposensitivity, difficulty with arousal, muted or absent orgasm.
Clitoral adhesions are common among female patients with lichen sclerosus, but also among the general population.
Vulvodynia’s cause of disease is highly idiopathic.
Pain confined to the vulval vestibule, known as vestibulodynia, has at least three known sub-types:neuroproliferation, hormonally-mediation, and inflammation.
Neuroproliferation can be present from birth or acquired later in life.
Hormonally-mediated vestibulodynia can be caused by hormonal medications like oral birth control.
Inflammatory vestibulodynia can develop as part of an immune response.
Possible causes of vulvodynia include Sjögren syndrome, the symptoms of which include chronic vaginal dryness, genetic predisposition to inflammation, allergy or other sensitivity, an autoimmune disorder similar to lupus erythematosus or to eczema or to lichen sclerosus, infections such as yeast infections, bacterial vaginosis, HPV, HSV,injury, and neuropathy.
Some cases are due to negative outcomes of genital surgery, such as a labioplasty.
Initiation of hormonal contraceptives that contain low- dose estrogen before the age of 16 could predispose women to vulvar vestibulitis syndrome.
A significantly lower pain threshold in the vestibulum, has also been associated with the use of hormonal contraceptives in women.
Pelvic floor dysfunction may be the underlying cause of some women’s pain.
Many co-morbidities are commonly associated with vulvodynia: fibromyalgia, irritable bowel syndrome, interstitial cystitis, pelvic floor dysfunction, endometriosis, depression and anxiety disorders.
Diagnosis:
The diagnosis is based on the typical complaints of the patient, essentially normal physical findings, and the absence of identifiable causes per the differential diagnosis.
Patients often will describe the touch of a cotton ball as extremely painful
The vagina should be examined, and tests, including wet mount, vaginal pH, fungal culture, and Gram stain, should be performed as indicated.
Only about half of the women who meet the criteria for vulvodynia will seek medical help, and many will see several doctors before a correct diagnosis is made.
Less than 2% of the people with vulvodynia who seek help obtain a diagnosis.
Affected women are also often hesitant to seek treatment for chronic vulvar pain, especially those who begin experiencing symptoms around the same time they become sexually active.
Many patients have been told that the pain is “in their head”.
Differential diagnosis:
Infections: urinary tract infection, candidiasis, herpes, HPV, vaginitis
Dermetological diseases: lichen sclerosus, lichen
Neoplasm: Paget’s disease, vulvar carcinoma
Neurologic disorder: neuralgia secondary to herpes virus, spinal nerve injury, pudendal nerve entrapment
Treatment: none are uniformly effective.
Treatments include:
Medications:
Creams and ointments containing lidocaine, estrogen or tricyclic antidepressants.
Antidepressants and anticonvulsants.
Injectable medications included steroids and botulinum toxin have been tried with limited success.
Physical therapy Pelvic floor physical therapy may help treat the pelvic floor dysfunction and help the patient gain greater control over their pelvic floor muscles.
Vestibulectomy surgery remove the vulval vestibule, and it may be suggested as a first-line treatment for neuroproliferative vestibulodynia.
It is often only offered after conservative measures have failed.
Lifestyle changes are often recommended such as not using underwear, that may irritate the area, and using lubricant during sex.
The percentage of women affected is estimated to range between 10-28%.
Vulvar pain is a quite frequent complaint in women’s health clinics.
