 Thymoma with immunodeficiency, Good’s syndrome, is a rare disorder that occurs in adults in whom hypogammaglobulinemia, deficient cell-mediated immunity, and thymoma may develop almost simultaneously.
Thymoma with immunodeficiency, Good’s syndrome, is a rare disorder that occurs in adults in whom hypogammaglobulinemia, deficient cell-mediated immunity, and thymoma may develop almost simultaneously.
The cause of Good Syndrome is unknown, but is thought to be an autoimmune process affecting the bone marrow.
Most patients present with an immunodeficient state and recurrent sinopulmonary infections in their 4th or 5th decade of life.
The immunodeficiency abnormalities may occur before or after the diagnosis of a thymoma.
It is an immunodeficiency involves both deficient humoral and cellular immunity, with low total serum antibodies.
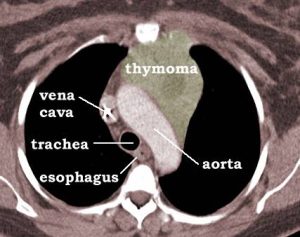
The thymoma may inhibit the thymus’s normal role to produce self-tolerant T lymphocytes.
These T-lymphocytes then attack the B cell precursors in the marrow, preventing maturation and ultimately resulting in hypogammaglobulinemia.
Thymoma is characterized by increased susceptibility to bacterial, viral, and fungal infections.
Good Syndrome is associated with other autoimmune conditions including pure red cell aplasia and myasthenia gravis.
No formal diagnostic criteria exist.
It is defined as an adult-onset primary immunodeficiency associated with thymoma, hypogammaglobulinemia, diminished B and T cells, and inverted CD4/CD8+ ratio.
Treatment consists of thymectomy and immunoglobulin replacement with intravenous immunoglobulins.
Immunodeficiency, however, does not resolve after thymectomy.
Pneumococcal, meningococcal, and Hepatitis B vaccination is recommended in those with diminished humoral and cell-mediated immunity.
There are advocates for prophylaxis with trimethoprim-sulfamethoxazole if CD4 counts are lower than 200 cells/mm^3.
