 Thrombectomy is the removal of a thrombus under angiographic guidance.
Thrombectomy is the removal of a thrombus under angiographic guidance.
It has become an excepted treatment for acute ischemic stroke caused by occlusion of a large cerebral vessel.
In patients with acute stroke, and a large infarct of unrestricted size, thrombectomy plus medical care, results in better, functional outcomes and lower mortality in medical care alone, but leads to a higher incidence of symptomatic intracerebral hemorrhage.
Endovascular thrombectomy is an interventional procedure of removing a blood clot from a blood vessel.
It is commonly performed in the cerebral arteries.
It is now a widespread procedure performed in most primary thrombectomy capable, or comprehensive stroke centers.
Mechanical thrombectomy is a safe and effective treatment for individuals who have an acute ischemic stroke out to 24 hours of symptom onset.
Thrombectomy for the treatment of acute ischemic stroke, due to large vessel occlusions, has been demonstrated irrefutably by clinical trials.
Clinical trials have established that endovascular thrombectomy superior in patients with large ischemic core volume of 50 mL or greater.
Cerebral ischemia injury, results from an imbalance of cerebral blood, flow and energy demand, leading to irreversible infarction.
Severely injured as to be irretrievably destined to infarct is defined as ischemic core, while ischemic penumbra refers to tissue that remains temporary viable, but is hypoperfused below level that allows for neurological function.
Such penumbral tissue goes on to infarct, if not timely, reperfused
The procedure is performed with general anesthesia or under conscious sedation.
Coaxial catheters are pushed inside the arterial circulation, usually through a percutaneous access to the right femoral artery, and a microcatheter is finally positioned beyond the occluded segment.
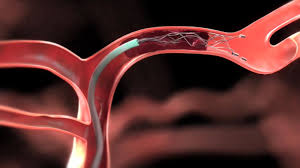
A stent-retriever is deployed to catch the thrombus.
The stent is pulled out from the artery, usually under continuous aspiration in the larger catheters.
Direct aspiration is performed by pushing a large soft aspiration catheter into the occluded brain vessel and applying direct aspiration to retrieve the thrombus; it can be combined with the stent-retriever technique to achieve higher recanalization rates.
Treatment guidelines have included the use of intravenous alteplase preceding thrombectomy, if there are no contraindications to its use.
The use of bridge intervenous thrombolysis before thrombectomy in acute stroke due to the occlusion of a large cerebral vessel remains the main therapeutic option.
In patients presenting at thrombectomy, capable stroke centers, the benefit with intravenous thrombolysis plus thrombectomy, versus thrombectomy alone is time dependent, and statistically significant only if the time from symptom onset to expected administration of intravenous thrombolysis is short-within-2hrs20 minutes(Kaesmacher J).
CHOICE study demonstrated the use of Alteplase following thrombectomy is more effective than Alteplase alone in Acute ischemic stroke.
Large vessel occlusion strokes can be efficaciously treated among carefully selected patients of approximately 3 to 7 for regaining independence.
Among patients with acute ischemic stroke, due to large vessel occlusion undergoing endovascular thrombectomy, the addition of methylprednisolone did not significantly improve the degree of overall disability (MARVEL trial).
In the TESLA randomized clinical trial among patients with a large infarct of the brain on noncontrast CT within 24 hours, did not demonstrate improvement in functional outcomes at ninety days (TESLA Investigators).
In patients with acute ischemic stroke due to large vessel occlusion presenting within 24 hours of time last known to be well, and who had achieved near complete to complete reperfusion with endovascular reperfusion thrombectomy, adjunctive intra-arterial tenecteplase did not significantly increase the likelihood of freedom from disability at 90 days (POST-TNK investigators).
Among patients with acute ischemic stroke due to large vessel, occlusion, adjunct intra-arterial urokinase after near complete or complete reperfusion by endovascular thrombectomy did not significantly increase the likelihood of survival without disability at 90 days (POST-UK investigators).
