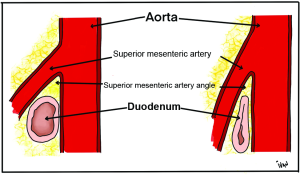
 Superior mesenteric artery (SMA) syndrome is an uncommon clinical entity characterized by compression of the third, or transverse, portion of the duodenum between the aorta and the superior mesenteric artery.
Superior mesenteric artery (SMA) syndrome is an uncommon clinical entity characterized by compression of the third, or transverse, portion of the duodenum between the aorta and the superior mesenteric artery.
Causes chronic, intermittent, or acute complete or partial duodenal obstruction.
Reported incidence 0.1-0.3%, with 0.013-0.78% of barium upper GI studies suggesting the diagnosis.
A complication of scoliosis surgery, anorexia, and trauma.
A diagnosis of exclusion.
The superior mesenteric artery commonly forms an angle of approximately 45° with the abdominal aorta.
The third part of the duodenum crosses caudal to the origin of the superior mesenteric artery, coursing between the superior mesenteric artery and aorta.
Mechanical factors that narrows the aorta-mesenteric angle to approximately 6-25° can cause entrapment and compression of the third part of the duodenum as it passes between the superior mesenteric artery and aorta, resulting in superior mesenteric artery syndrome.
The aorta-mesenteric distance in superior mesenteric artery syndrome is decreased to 2-8 mm from 10-20 mm.
Other possible causes include high insertion of the duodenum at the ligament of Treitz, and the compression of the duodenum due to peritoneal adhesions.
The syndrome can result in impaired nutrition, dehydration, electrolyte abnormalities, obstructing duodenum, GI bleeding , and gastric perforation.
More females are affected with a 3:1 ratio to males.
Average age at onset about 40 years.
Usually occurs in older children and adolescents.
Patients often present with chronic upper abdominal symptoms such as epigastric pain, nausea, eructation, vomiting, postprandial discomfort, early satiety, and sometimes, subacute small bowel obstruction.
Symptoms often develop from 6-12 days after scoliosis surgery.
The symptoms are typically improved in the left lateral decubitus, prone, or knee-to-chest position.
Typically symptoms worsened in the supine position.
These maneuvers alter the small bowel mesenteric tension at the aortomesenteric angle.
An asthenic habitus is noted in about 80% of cases.
Peptic ulcer disease has been noted in 25-45% of the patients, and hyperchlorhydria has been noted in 50%.
Etiologic factors that may precipitate narrowing of the aortomesenteric angle and recurrent mechanical obstruction include: spinal disease, deformity, spinal trauma and spinal corrective surgery, postoperative weight loss, rapid linear growth without compensatory weight gain, particularly in adolescents,
Adolescents with low body mass index may be at higher risk for developing SMA syndrome after spinal fusion for scoliosis than patients with a higher body mass index.
Unusual and rare causes include traumatic aneurysm of the superior mesenteric artery, abdominal aortic aneurysms, mycotic aortic aneurysms, and familial superior mesenteric artery syndrome,
The diagnosis remains difficult, and confirmation usually requires radiographic studies.
Diagnostic imaging include: upper GI series, hypotonic duodenography, and CT scanning.
Radiographic findings on fluoroscopic examination may include dilation of the first and second portions of the duodenum with marked narrowing at the third portion.
Other findings include delayed gastroduodenal emptying, and antiperistaltic waves proximal to the obstruction, and relief of the obstruction by a change to the left lateral decubitus position.
Relief of the obstruction may also be obtained by applying pressure below the umbilicus in the cephalad and dorsal direction, elevating the root of the small bowel mesentery by a procedure known as the Hayes maneuver.
CT scanning of the abdomen can provide diagnostic information, including aorta-superior mesenteric artery distances, findings of duodenal distension, and can assess intra-abdominal and retroperitoneal fat, identify compression of the left renal vein, abdominal aortic aneurysm and portal vein abnormalities.
CT criteria include an aortomesenteric angle of less than 22 degrees (less than 22 degrees in children) and an aortomesenteric distance of less than 8-10 mm.
Abdominal ultrasonography may be helpful in measuring the angle of the superior mesenteric artery and the aortomesenteric distance, and with endoscopy may allow diagnosis, avoiding other tests with radiation exposure.
Conservative initial treatment is recommended in all patients, as reversing or removing precipitating factors is usually successful management in the SMA syndrome.
Proper treatment includes providing nutritional support by enteral or parenteral means, nasogastric decompression, and positional changes after feeding to the left lateral decubitus position, prone, knee-to-chest position.
Enteral feeding may be done via a jejunostomy tube.
As the process resolves the patient can be started on oral liquids followed by slow and gradual introduction of small and frequent soft meals, until regular solid foods are introduced.
In acute cases medical management Is highly successful, and conservative treatment should be instituted for at least 4-6 weeks prior to considering surgical intervention.
If conservative measures are not effective, particularly in patients with prolonged history of weight loss, duodenal dilatation and stasis, and complications of peptic ulcer disease, surgical intervention should proceed.
Surgical options include a duodenojejunostomy or gastrojejunostomy to bypass the obstruction or a duodenal derotation procedure to alter the aortomesenteric angle.
The latter procedure places the third and fourth portions of the duodenum to the right of the superior mesenteric artery, and is best reserved for pediatric patients in whom the superior mesenteric artery syndrome may be related to congenital anatomic conditions that predispose to their symptomatology.
Surgical duodenal derotation usually requires a laparotomy, but may be done laparoscopically, with duodenal mobilization after division of the ligament of Treitz.
With a duodenojejunostomy, the prototypical surgical treatment, the compressed portion of the duodenum is released and an anastomosis is created between the duodenum and jejunum anterior to the superior mesenteric artery.
A gastrojejunostomy is reserved for patients who have contraindication to a duodenojejunostomy, including duodenal ulcer disease or severe stomach and duodenum are dilation.
Metoclopramide may be used to provide a prokinetic GI effect.
Metoclopramide is a dopamine antagonist that stimulates acetylcholine release in the myenteric plexus, and also acts centrally on chemoreceptor triggers in the floor of the fourth ventricle, providing antiemetic activity.
Complications of the syndrome include: lectrolyte imbalance, metabolic alkalosis, dehydration, malnutrition, impaired urine output, hypotension, aspiration, and peptic ulcer disease.
Prognosis is excellent if diagnosis is timely and the patient receives appropriate therapy.
Mesenteric ischemia secondary to septic emboli is a rare complication of infective endocarditis.
Diagnosis of a superior mesenteric embolus can be made with ultrasound, CT angiography or MRI of the abdomen.
