 2379
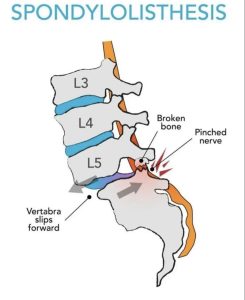
2379Slipping forward of one lumbar vertebra on another with an intact neural arch.
Degenerative spondylolisthesis is acondition in which one vertebrae has stepped forward in relation to the next lower vertebrae.
Rare before the age of 50 years.
Patients are usually older than 60 years, and typically have leg and back pain and restricted function due to lumbar spinal stenosis caused by the spondylolisthesis, disc bulging, and ligamentous and facet hypertrophy.
Spondylolisthesis, is much more common in women than in men:
a vertebra slips forward on the one below it, misaligning the spinal column.
Disproportionately affects females, particularly black women with a male:female ratio of 1:6.
Spondylolisthesis-slippage most commonly occurs at the L4-L5 level and rarely exceeds 30% of vertebral width.
Generally asymptomatic.
Can be associated with spinal stenosis.
Refers to the forward or anterior displacement of one vertebra over another.
Commonly involves the fifth lumbar vertebra.
Backward displacement is referred to as retrolisthesis.
A hangman’s fracture is a specific type of spondylolisthesis where the second cervical vertebra (C2) is displaced anteriorly relative to the C3 vertebra due to fractures of the C2 vertebra’s pedicles.
Symptoms include:
Stiffening of the back and a tightening of the hamstrings, with a resulting change in both posture and gait.
A leaning-forward or semi-kyphotic posture, due to compensatory changes may be seen.
In more advanced causes, waddling due to compensatory pelvic rotation due to decreased lumbar spine rotation, may be seen.
This alteration in gait is often associated with atrophy in the gluteal muscles due to lack of use.
Generalized lower-back pain may occur, with intermittent shooting pain from the buttocks to the posterior thigh, and/or lower leg via the sciatic nerve.
Coughing and sneezing can intensify the discomfort.
Tingling and numbness may occur.
Some patients experience a slipping sensation when moving into an upright position.
Sitting and standing up may be painful and difficult.
It can be categorized by cause, location and severity.
Degenerative spondylolisthesis, known as type 3, is a disease of the older adult that develops as a result of facet arthritis and joint remodeling.
Slippage of a vertebra may result from joint arthritis and ligamentum flavum weakness.
Degenerative forms of spondylolisthesis are more likely to occur in older women, persons and African Americans.
Traumatic spondylolisthesis is rare and is a result of acute fractures in the neural arch.
Type 1 dysplastic spondylolisthesis results from congenital abnormalities of the upper sacral facets or inferior facets of the fifth lumbar vertebra, and accounts for 14% to 21% of all spondylolisthesis.
Isthmic spondylolisthesis, which is type 2, is caused by a defect in the pars interarticularis but it can also be seen with an elongated pars.
Pathologic spondylolisthesis, known as type 5, is caused by either infection or a malignancy.
Post-surgical/iatrogenic spondylolisthesis, type type 6, is caused by complications after surgery.
Spondylolisthesis is characterized by the location of which vertebrae are involved, and may also specify which parts of the vertebrae are affected.
Isthmic spondylolisthesis with a defect in the pars interarticularis is the most common form of spondylolisthesis.
Isthmic spondylolisthesis, also called spondylolytic spondylolisthesis, occurs with a reported prevalence of 5–7 percent in the US population.
A slip or fracture of the intravertebral joint is usually acquired between the ages of 6 and 16 years
Roughly 90 percent of these isthmic slips are low-grade and 10 percent are high-grade.
A: pars fatigue fracture
B: pars elongation due to multiple healed stress effects
C: pars acute fracture
With symptomatic isthmic spondylolisthesis conservative treatment is offered initially with activity modification, pharmacological intervention with NSAIDs, and a physical therapy.
With severe radicular component a short course of oral steroids can be considered.
Epidural steroid injections, either interlaminal or transforaminal, performed under fluoroscopic guidance can help with severe radicular pain.
Lumbosacral orthoses may be of benefit for some patients.
Degenerative spondylolisthesis with spinal stenosis is one of the most common indications for spine surgery
Typically a laminectomy is performed, with minimally invasive and open surgical techniques.
Randomized controlled trials investigating the benefit of adding fusion to decompression in patients with lumbar spondylolithesis: fusion does not have value for this patient group.
In the NORSTEN-DS clinical trial patients who underwent surgery for a degenerative lumbar spondylolithesis, decompression alone was not inferior to decompression with instrumented fusion over a period of two years.
