 Salivary gland neoplasms arise in the salivary glands are relatively rare.
Salivary gland neoplasms arise in the salivary glands are relatively rare.
Represent both benign and malignant subtypes.
Make up 6% of all head and neck tumors.
Include adenoidcystic carcinoma, mucoepidermoid carcinoma, and salivary duct carcinoma.
Incidence of salivary gland neoplasms is approximately 1.5 cases per 100,000 individuals in the United States.
An estimated 700 deaths related to salivary gland tumors occur annually.
Most commonly appear in the sixth decade of life.
Patients with malignant lesions typically present after age 60 years.
Patients with benign lesions usually present when older than 40 years.
Benign neoplasms occur more frequently in women.
Malignant tumors are distributed equally between the sexes.
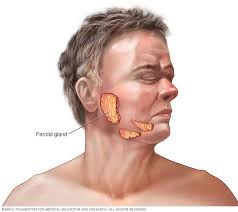
Divided into 2 groups: the major salivary glands and the minor salivary glands.
The major salivary glands consist of the following 3 pairs of glands: the parotid glands, the submandibular glands, and the sublingual glands.
The minor salivary glands comprise 600-1000 small glands distributed throughout the upper aerodigestive tract.
80% arise in the parotid glands, 10-15% arise in the submandibular glands, and the remainder arise in the sublingual and minor salivary glands.
About 80% of parotid neoplasms are benign, with the relative proportion of malignancy increasing in the smaller glands.
As the size of the gland decreases, the incidence of malignancy of a tumor in the gland increases.
The most common tumor of the parotid gland is the pleomorphic adenoma, which represents about 60% of all parotid neoplasms.
Almost half of all submandibular gland tumnors and most sublingual and minor salivary gland tumors are malignant.
Rare in children, with most tumors (65%) being benign.
Hemangiomas are the most common salivary gland tumors in children, followed by pleomorphic adenomas.
35% of salivary gland neoplasms in children are malignant and mucoepidermoid carcinoma is the most common type.
Salivary duct carcinoma has a poor prognosis, but is quite rare.
Low dose radiation therapy is associated with the development of parotid neoplasms 15-20 years after treatment,wit an increased incidence of pleomorphic adenomas, mucoepidermoid carcinomas, and squamous cell carcinomas.
Malignant lesions not associated with tobacco and alcohol, and occupational exposure to silica dust and nitrosamines.
Tobacco smoking has been associated with the development of Warthin tumors.
Oncogenes associated include p53, Bcl-2, PI3K/Akt, MDM2, and ras, and vascular endothelial growth factor is expressed by over half of salivary gland carcinomas and is correlated with clinical stage, recurrence, metastasis, and survival.
Seventy percent of pleomorphic adenomas have associated chromosomal rearrangements, and the loss of chromosomal arms 2q, 5p, 12p, and 16q more than 50% of the time.
In mucoepidermoid carcinoma, the t(11;19)(q21;p13) chromosomal translocation is present in up to 70% of cases, which results in the production of a fusion protein associated with longer median survival and lower rates of local recurrence and distant metastases.
CD117, or c-kit, a tyrosine kinase receptor is found in adenoid cystic carcinoma, myoepithelial carcinoma, and lymphoepithelioma-like carcinomas.
Loss of chromosomal arm 19q has been reported to occur commonly in adenoid cystic carcinoma.
Most patients present with a slowly enlarging painless mass.
Parotid neoplasms most commonly occur in the tail of the gland, and of the parotid gland can be treated with superficial parotidectomy.
Monomorphic adenomas are benign, slow growing, and the least aggressive of the salivary gland tumors, and represent fewer than 2% of salivary gland neoplasms.
Most common variety of monomorphic adenoma is the basal cell adenoma, which occurs most commonly in the minor salivary glands, usually the upper lip.
Basal cell adenoma of the major salivary glands usually involves the parotid gland.
Basal cell adenoma treatment consists of surgical excision with a margin of normal tissue.
Mucoepidermoid carcinoma is the most commonly occurring malignant neoplasm of the parotid gland.
Mucoepidermoid carcinoma is the second most common malignant neoplasm of the submandibular gland after adenoid cystic carcinoma.
Mucoepidermoid carcinoma represents approximately 8% of all parotid tumors.
Mucoepidermoid carcinomas are divided into low, intermediate, and high grade lesions.
Mucoepidermoid carcinomas contain 2 types of cells, mucous and epidermoid cells.
Low-grade mucoepidermoid carcinomas tumors have a higher preponderance of mucous cells than epidermoid cells do.
The ratio of epidermoid cells rises in higher grades.
High-grade mucoepidermoid carcinomas resemble squamous cell carcinomas.
Low-grade mucoepidermoid carcinomas tumors are usually small, partially encapsulated and may have some cystic components.
High-grade mucoepidermoid carcinomas tumors are usually large, infiltrative without an apparent capsule.
Low-grade tumors contain sheets of mucoid cells separated by bands of epidermoid cells.
High-grade mucoepidermoid carcinomas are composed of malignant epidermoid cells.
High-grade mucoepidermoid carcinoma can be differentiated from squamous cell carcinoma by staining for the presence of mucous cells.
Adenoid cystic carcinoma is the second most common malignant salivary gland tumor, representing approximately 6% of all salivary gland neoplasms.
Adenoid cystic carcinoma are characterized by prolong progression and multiple occurrences.
Adenoid cystic carcinomaIt is the most common malignancy in the submandibular gland.
Adenoid cystic carcinoma usually presents a slow-growing painless mass, and uncommonly metastasizes to regional lymph nodes.
Adenoid cystic carcinoma more frequently associated with distant metastasis than regional nodal involvement.
Adenoid cystic carcinoma associated with lung metastases.
Adenoid cystic carcinoma 5 year survival is approximately 65%.
Adenoid cystic carcinoma 15-year survival is only 12%, indicating the slow growth of this tumor.
Adenoid cystic carcinoma associated with local recurrences, with a tendency to grow along perineural and perivascular planes.
Adenoid cystic carcinoma associated with skip lesions.
Adenoid cystic carcinoma grossly, appear as monolobular and nonencapsulated.
Adenoid cystic carcinoma appear microscopically as basaloid epithelial elements that form cylindrical structures, and classified as cribriform, tubular, and solid patterns.
All histologic patterns are associated with perineural extension accounting for the difficulty in eradicating adenoid cystic carcinoma.
Acinic cell carcinoma is a low-grade neoplasm that represents 1% of all salivary gland neoplasms, with almost 95% arising in the parotid gland, and most of the remainder arise in the submandibular gland.
Acinic cell carcinoma lesions involve serous cells.
Carcinoma ex-pleomorphic adenoma are lesions that arises from a preexisting pleomorphic adenoma and contains only malignant epithelial elements.
Carcinoma ex-pleomorphic adenoma account for 2-4% of salivary gland malignancies, and manifest as a sudden rapid growth of an otherwise slow growing or stable mass.
Carcinoma ex-pleomorphic adenoma may appear as an adenocarcinoma, squamous cell carcinoma, or undifferentiated carcinoma.
Carcinoma ex-pleomorphic adenoma behave aggressively and are associated with a poor prognosis, and associated with common regional and distant metastases.
Squamous cell carcinoma of the salivary glands is rare, and high-grade mucoepidermoid carcinoma must be ruled out as must metastatic squamous cell of the skin or lung.
Primary squamous cell carcinomas likely represent 0.3-1.5% of salivary gland tumors.
Adenocarcinomas of the salivary gland are rare, making up approximately 2-3% of salivary gland tumors.
Adenocarcinomas of the salivary gland have an aggressive biologic behavior.
Cytoplasmic immunostaining for pRb or p130, a member of the Rb family of tumor suppressor genes, is correlated with increased tumor grade
The loss of immunostaining for p63 in myoepithelial cells has been associated with malignancy and loss of differentiation.
Mucoepidermal cancer uniquely expresses MUC5AC but not MUC3
Adenoid cystic cancer expresses MUC3 and not MUC5AC.
Polymorphous low-grade adenocarcinoma (PLGA) is an indolent tumor that has a predilection for perineural invasion and is predominantly a tumor of minor salivary glands with a ow rate of cervical metastasis.
Polymorphous low-grade adenocarcinoma (PLGA) has a good prognosis with a 10 year survival of greater than 90%, and therefore postoperative radiation does not improve survival.
Salivary duct carcinoma is rare aggressive tumor that usually arises from the parotid gland and represents 1-3% of all salivary gland malignancies .
Salivary duct carcinoma predominantly affects men and in the 7th decade and is associated with high rates of cervical nodal metastases with more than 50% having such disease at the time of diagnosis.
Salivary duct carcinoma associated with a poor prognosis and the five-year survival estimated to be 42% stage I and 23% for stage IV disease
Salivary duct carcinoma metastases occur equally between local and distant lesions.
Salivary duct carcinoma is treated with parotidectomy and ipsilateral neck dissection and postoperative radiation, although the ;atter efficacy is unknown.
Surgical principles for parotid tumors is that incisional biopsies and enucleation are not appropriate procedures, and superficial parotidectomy with identification and dissection of the facial nerve is the minimum operation for diagnosis and treatment of parotid masses.
Surgery is the primary treatment of malignant tumors of the salivary glands aznd is often combined with postoperative radiation therapy, depending on the specific tumor characteristics and stage.
The extent of surgical resection is based on the size of the tumor, local extension, and neck metastases, and the facial nerve is spared unless it is directly involved by the lesion.
Postoperative radiation therapy is recommended for all but small low-grade tumors.
To acquire the histopathologic diagnosis of parotid masses the minimum procedure is a superficial parotidectomy with identification and preservation of the facial nerve.
The shift from previous enucleation to superficial parotidectomy as the minimal procedure for parotid tumors has substantially reduced recurrence rates for both benign and malignant disease.
The facial nerve should not be sacrificed for benign tumors.
On the basis of the histologic classification and clinical stage four groups of salivary gland tumors can be categorized.
Group 1 includes T1 and T2 low-grade tumors such as a low-grade mucoepidermoid carcinoma, acinic cell carcinoma which are managed by parotidectomy, superficial or total, with an adequate margin of normal tissue, preservation of the facial nerve and examination of first-echelon nodes.
For group 1 lesions uncomplicated resection, with negative nodes does not require radiation therapy.
Group 2 lesions includes T1 and T2 tumors with high-grade features such as high-grade mucoepidermoid carcinoma, adenoid cystic carcinoma, squamous cell carcinoma, adenocarcinoma, carcinoma ex-pleomorphic adenoma.
Group 2 lesions are treated with total parotidectomy, including the first level lymph nodes, and these upper lymph nodes are positive for tumor further neck dissection is required.
Group 2 salivary tumor management should preserve the facial nerve unless it is directly infiltrated by tumor. If the facial nrve is involved the nerve is resected until clear margins, and it is reconstructed with cable grafting.
Group 2 salivary tumor management includes postoperative radiation therapy to the parotid region and neck.
Group 3 salivary gland tumors include any T3 tumor, any N+, and any recurrent tumors not in group 4.
Group 3 salivary gland tumors require radical parotidectomy with sacrifice of the facial nerve in order to obtain sufficient tumor-free margins, reconstruction of the facial nerve with cable graft, neck dissection and postoperative radiation therapy.
Group 4 includes T4 tumors.
For group 4 tumors radical parotidectomy with excision of the involved structures as needed to obtain tumor-free margins, neck dissection for nodal positive disease and postoperative radiation therapy should be administered.
Submandibular gland tumor masses are subjected to fine needle aspiration biopsy (FNAB) to rule out inflammatory disease and metastatic disease.
Benign neoplasms of the submandibular gland require complete excision of the gland while malignant neoplasms require complete excision of the gland plus extended surgery.
Malignant submandibular salivary gland malignancies are treated similarly as parotid gland malignancies.
Submandibular salivary gland malignant tumors which are small and low grade -group 1 require submandibular triangle excision without resection of cranial nerves.
For group 2 malignant mandibular tumors, a wider resection of the submandibular triangle is required for clear margins, nerves are sacrificed nerves if they are involved with a tumor, and neck dissection is performed for nodal positive disease, and postoperative radiation is administered.
Group 3 tumors of the submandibular malignant tumors frequently require sacrifice of the lingual and hypoglossal nerves, along with radical neck dissection and postoperative radiation therapy.
Group 4 malignant submandibular tumors require wide surgical resection depending on extent of the tumor, including mandible, floor of mouth, tongue, skin, and cranial nerves, neck dissection and postoperative radiation therapy.
Salivary gland neoplasms respond poorly to chemotherapy, and adjuvant chemotherapy is not indicated.
Doxorubicin and platinum based agents and docetaxel, paclitaxel, mitoxantrone or vinorelbine, are the most commonly used chemotherapy agents.
Radiotherapy is considered for nonresectable disease.
Postoperative radiation in T1 and T2 parotid gland tumors increases 5-year disease-free survival from 70% to 92%.
Postresection radiotherapy for carcinoma ex pleomorphic adenoma associated with a 26% improvement in 5-year local control.
Prospective randomized controlled studies are needed to confirm the usefulness of postoperative radiotherapy.
Gamma-knife stereotactic radiosurgery, brachytherapy, neutron and photon radiation are being evaluated radiation treatments for salivary gland tumors.
For advanced stage disease 3 or 4 with invasion of bone, nerves or lymph nodes doses of radiation 60 Gy required postoperatively, and higher doses required if residual disease is present.
American Joint Committee for Cancer Staging and American Joint Committee for Cancer Staging and End Result Reporting (AJCC) classification of major salivary gland malignancies: The system includes tumor size, local extension of tumor, cervical lymph node metastases, and distant metastases.
The 5-year relative survival rate is 85% for stage I tumors, 66% for stage II tumors, 53% for stage III tumors, and 32% for stage IV tumors.
Low-grade tumors include acinic cell carcinoma and low-grade mucoepidermoid carcinoma.
High-grade tumors include adenoid cystic carcinoma, high-grade mucoepidermoid carcinoma, carcinoma ex-pleomorphic adenoma, squamous cell carcinoma, and adenocarcinoma.
Low-grade tumors have 10-year survival rates of 80-95%.
Hi-grade salivary gland tumors have 10-year survival rates that range from 25-50%.
High levels of Ki-67 found in tumors strongly correlated with poor survival.
In mucoepidermoid salivary gland carcinomas, immunostaining with increased MUC1 expression have increased tumor progression and worse prognosis, whereas increased MUC4 expression is associated with decreased progression and better survival.
Regional lymph node metastases is related to tumor histopathology and size.
The highest rates of lymph node metastases occur with high-grade salivary gland carcinomas: mucoepidermoid carcinoma, 44%, squamous cell carcinoma, 36%, adenocarcinoma 26% of cases, undifferentiated carcinoma 23% of cases, and carcinoma ex-pleomorphic adenoma 21% of cases.
Occult nodal metastases seen most commonly with squamous cell carcinoma , 40%, and high-grade mucoepidermoid carcinoma 16%.
Neck dissection is performed for clinically positive disease of the neck, but not electively.
Recurrence rates are, however, higher in patients without elective neck dissection and that the disease-free survival rate is significantly lower in patients without elective neck dissection.
Sentinel lymph node biopsies with the use of lymphoscintigraphy can be used intraoperatively to identify first level nodes.
Neck dissection may be appropriate in patients with a high probability of occult cervical metastases, with lymph nodes >4 cm) and with an increased risk of lymphatic spread.
Pain as a presenting symptom can be present in both malignant and benign disease.
Pain in the presence of malignancy is associated with a lower 5-year survival rate than those without pain.
Facial nerve involvement with parotid carcinoma is an independent risk factor for disease-free survival.
Parotid tumors with normal facial nerve function have a 69% chance of disease free survival compared with 37% with partially dysfunctional facial nerves and 13% with completely impaired function.
Distant metastases correlated with T and N stage, male sex, perineural invasion, histological type, and skin involvement.
Distant metastases manifest in 21% of patients with parotid tumors.
Rate of distant metastases among high-grade salivary gland tumors is 32%.
The distant metastasis rate is nearly 50% for adenoid cystic carcinomas,
The most common sites for metastases from salivary gland involve the lung and bone.
Patients with adenoid cystic carcinoma may survive longer than 10 years because of the slow growth of these tumors, however survival with metastatic disease is short.
5 year survival for adenoid cystic carcinoma with distant metastases is approximately 32% and in patients with acinic cell carcinoma, the survival rate with distant metastases is about 30% at 5 years.
With metastatic disease there is no evidence that cytotoxic chemotherapy impacts the natural history.
