 Characterized by neurological disturbances associated with predominant posterior cerebral circulation involvement.
Characterized by neurological disturbances associated with predominant posterior cerebral circulation involvement.
The incidence is reported to be 0.8% among patients with end-stage renal disease, approximately 0.7% among those with SLE, 0.5% among those of undergone solid organ, transplantation and from 20% to 98% among those with preeclampsia or eclampsia.
The incidence in children with similar medical difficulties is estimated to be .04%.
PRES occurs in all age groups, with the highest incidence among young and middle-aged adults.
It is more prevalent in women than among men.
The mean age is approximately 57 years and 72% are women and 68% are Caucasian.
Posterior reversible encephalopathy (PRES) is a radiographic syndrome characterized by headaches, altered consciousness, visual disturbances, and seizures associated with radiologic findings of edema involving bilateral parietal-occipital lobes (Hinchey J et al).
It is an acute or subacute cerebral syndrome.
It is associated with the white matter vasogenic edema, predominantly affecting the occipital and parietal lobes of the brain.
Cause remains elusive, but most common explanation is quickly developing hypertension leading to an interruption of the cerebral autoregulation.
Hypotheses for underlying biologic changes of PRES include cerebral vascular dysregulation in cases of acute hypertension and cerebral vascular endothelial dysfunction in association with or after exposure to toxic agents.
The involvement of the occipital and posterior parietal lobes that characterize PRES may be attributable to less sympathetic innervation of the posterior cerebral areas in the anterior circulation.
The mechanism of injury is the cerebral vascular endothelium with disruption of the blood brain barrier leading to vasogenic edema.
It may manifest with headache, encephalopathy, seizures, or visual disturbances in various combinations.
It is typically associated with acute, severe hypertension, or moderate, but acute elevations in blood pressure outside of the custom range for the patient, or from the exposure to certain drugs and toxic agents, mostly from chemotherapy and immunosuppressive drugs.
Up to 94% of patients manifest a nondescript encephalopathy ranging from mild confusion to coma.
In up to half of the cases there is a dull and diffuse headache, but occasionally may be a sudden thunderclap headache.
General or partial seizures occur in approximately 3/4 of patients had some time in the course of PRES.
Seizures may progress to status epilepticus in up to 18% of patients.
Visual abnormalities a prominent and 20 to 39% of patients with diminished acuity, visual field defects, visual, neglect, visual, hallucinations, or blindness.
Less commonly focal paresis, incoordination, hyperreflexia, and spinal manifestations can occur.
In a retrospective series, the initial manifestation with seizures in half the patients, and vision loss with speech difficulty, in 1/5 of patients.
Drug and toxic exposures are probably related to cerebral vascular, dysregulation or endothelial dysfunction.
Can be correlated with medical illness, hypertension, and treatment with medications that cause immunosuppression.
Syndrome may not be always reversible.
The lesion may not be confined to the white matter or the posterior regions of the brain.
Not necessarily confined to the posterior white matter of the brain, but can be located in the frontal lobe, basal ganglia, cortex and brain stem.
The process is usually associated with hypertensive encephalopathy, eclampsia, renal failure, general anesthesia, immunosuppressants and chemotherapy agents.
Pathogenesis suggested to be related to endothelial dysfunction with direct toxicity on vasculature leading to capillary leakage and blood barrier blood brain barrier disruption triggering vasogenic edema.
Auto-regulatory failure and secondary vasodilatation as is seen in hypertensive encephalopathy is often cited as an underlying mechanism.
The posterior cerebral circulation tends to be more susceptible due to less sympathetic innervation of the vertebrobasilar vasculature, which leads to an increase in arterial pressure, acutely.
This explains why edema is seeing primarily in the posterior circulation in the syndrome.
Usually reversible within days to weeks.
Agents associated with this process include cisplatin, cytosine arabinoside, rituximab, bevacizumab, and gemcitabine.
Hypertension the most common associated feature.
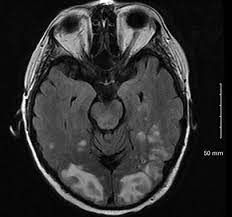
MRI hyperintense signals predominantly in the posterior hemispheres on T2 weighted images.
Most common neuroimaging abnormality is white matter vasogenic edema in the occipital and sometimes adjacent parietal lobes.
Wide spectrum of inflammatory disorders and medications such as chemotherapy and immunosuppressive agents.
Thought to be related to breakdown of the blood brain barrier with transudation of fluid and protein in the extra vascular space, with the result of cerebral edema.
Possibly secondary to cerebrovascular spasm and ischemia with secondary edema within the posterior brain circulation.
The most common neuroimaging abnormalities are in the parietal-occipital subcortical areas with T2 hyperintensity without enhancement.
Other areas of the brain such as the brainstem, cerebellum, frontal, and temporal lobes may be involved.
The abnormality seen on imaging primarily affect sub cortical white matter, however the cortex and basal ganglia may also be affected.
That edema can reverse completely and in a review of 53 cases total reversibility was seen in 58% of the cases and partial reversibility of the edema was seen in 26% (Liman TG et al).
The process can be triggered by an acute elevation of blood pressure, abnormal renal function, and immunosuppressive therapy.
Other triggering processes include eclampsia, transplantation, malignancy, chemotherapy, and acute or chronic renal disease.
In general, associated with hypertension and renal disorders.
Clinical manifestations include: seizures, headache, visual loss, altered mental status, and radiological alterations detected on MRI imaging of the brain.
Early recognition is important, as ischemia and hemorrhage may result, with permanent deficits if not treated promptly.
Neuroimaging is the essential diagnostic feature of PRES.
Edema is seen in the bilateral cerebral regions supplied by the posterior circulation and is readily evident on noncontrast CT of the brain.
MRI is preferred over CT because fluid attenuation inversion recovery and T2 weighted sequence is sensitive to vasogenic edema.
MRI signal changes occur, mostly in the bilateral white matter regions, and typically in the occipital lobes, but unilateral or gray matter, involvement and other patterns have been seen.
Additional imaging changes have been seen in the parietal occipital region, temporal region, frontal region, thlamic region, cerebellar region, brainstem region, and basal ganglia region.
Differential diagnosis of PRES: cerebral infarction, posterior circulation strokes, CNS infections, demyelinating diseases, brain cancer, dural venous thrombosis, CNS vasculitis, toxic and cephalopathies and mitochondrial disorders.
Management:
prompt control of the precipitating cause of PRES and supportive care are essential.
Up to 70% of patients, and especially those with severe hypertension, depressed, level of consciousness, or seizures are admitted to an ICU.
Treatment is directed at controlling the hypertension, managing seizures, brain, edema, and discontinuing or replacing precipitating factors.
In patients who have PRES without hypertension the associated medical or triggering agents need to identified and treated.
The prognosis is good with appropriate management.
Most patients recover within two weeks, however, poor outcomes in death have been reported.
Poor outcome is associated with brain hemorrhage and cytotoxic edema on imaging studies, whereas favorable outcomes are associated with preeclampsia and eclampsia.
