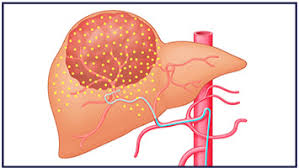
 A minimally invasive procedure that combines embolization and radiation therapy to treat liver cancer.
A minimally invasive procedure that combines embolization and radiation therapy to treat liver cancer.
Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer.
It is generally used with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver.
The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor.
TARE involves the direct insertion of radioactive microspheres to a region, resulting in a local and targeted deposition of radioactive dose.
Due to the local deposition, SIRT is regarded as a type of locoregional therapy.
Tiny glass or resin beads filled with the radioactive isotope yttrium Y-90 are placed inside the blood vessels that feed a tumor, blocksing the supply of blood to the cancer cells and delivers a high dose of radiation to the tumor while sparing normal tissue.
Can help extend the lives of patients with inoperable tumors and improve their quality of
The liver has a dual blood supply system; hepatic artery and the portal vein.
The healthy liver tissue is mainly perfused by the portal vein, while most liver malignancies derive their blood supply from the hepatic artery.
Transarterial chemoembolization or radioembolization, can selectively be administered in the arteries that are supplying the tumors and will preferentially lead to deposition of the particles in the tumor, while sparing the healthy liver tissue from harmful side effects.
Malignancies, including primary and many metastatic liver cancers are leading to preferential deposition of particles in the tumors.
Patients with minimal exposure to chemotherapy and low hepatic tumor burden with colorectal cancer have a better overall survival with radioembolization with ytrium-90 (Abbott AM et al).
TARE can be performed using several techniques, including whole liver treatment, lobar or segmental approaches.
Whole liver SIRT targets the entire liver in one treatment and can be used when the disease is spread throughout the liver.
Radiation lobectomy targets one of the two liver lobes: a good treatment option when only a single lobe is involved or when treating the whole liver in two separate treatments, one lobe at the time.
Radiation segmentectomy, is a technique where a high dose of radiation is delivered in one or two liver segments only,resulting in eradication of the tumor while damage to healthy liver tissue is contained to the targeted segments only.
Candidates for radioembolization include patients with:
Unresectable liver cancer of primary or secondary origin, such as hepatocellular carcinoma and liver-metastases: colorectal cancer, breast cancer, neuroendocrine cancer,cholangiocarcinoma or soft tissue sarcomas.
No response or intolerance to regional or systemic chemotherapy
No eligibility for potentially curative options such as radiofrequency ablation.
It is currently considered as a salvage therapy.
It has been shown to be safe and effective in patients for whom surgery is not possible, and chemotherapy was not effective.
SIRT, when added to first line therapy for patients with metastases of colorectal cancer, there was no superiority of SIRT over chemotherapy in terms of progression-free or overall survival.
SIRT is generally better tolerated than systemic therapy, with less severe adverse events.
For HCC patients SIRT can sometimes be used to decreases tumor size allowing patients to be candidates for curative treatment-bridging therapy.
When comparing SIRT with transarterial chemoembolization (TACE), several studies have shown favorable results for SIRT, such as longer time to progression, higher complete response rates and longer progression-free survival.
There are three types of commercially available microsphere for SIRT: Two of these use the radionuclide yttrium-90 (90Y) and are made of either glass (TheraSphere) or resin (SIR-Spheres).
The third type uses holmium-166 (166Ho) and is made of poly(l-lactic acid).
The therapeutic effect of all types radionuclides is based on local deposition of radiation dose by high-energy beta particles.
All three types of microsphere are permanent implants and stay in the tissue even after radioactivity has decayed.
90Y, a pure beta emitter, has half-life 2.6 days, or 64.1 hours.
166Ho emits both beta and gamma rays emitter, with half-life 26.8 hours.
Both 90Y and 166Ho have mean tissue penetration of a few millimeters.
90Y can be imaged using SPECT and positron emission tomography (PET).
166Ho’s additional gamma emission (81 KeV, 6.7%) makes 166Ho microspheres quantifiable using a gamma camera.
Theraspheres (glass 90Y microspheres) are FDA approved under a humanitarian device exemption for hepatocellular carcinoma (HCC).
SIR-spheres (resin 90Y microspheres) are FDA approved under premarket approval for colorectal metastases in combination with chemotherapy.
Contrast computed tomography and/or contrast-enhanced magnetic resonance imaging of the liver is required to assess tumor and normal liver volumes, portal vein status, and extrahepatic tumor burden.
Patients with irreversibly elevated serum bilirubin, AST and ALT are excluded, as these are markers of poor liver function.
Hepatic artery technetium (99mTc) macro aggregated albumin (MAA) scan is performed to evaluate hepatopulmonary shunting: Therapeutic radioactive particles travelling through such a shunt can result in a high absorbed radiation dose to the lungs, possibly resulting in radiation pneumonitis.
Initial angiographic evaluation includes: an abdominal aortogram, Superior mesenteric and Celiac arteriograms, and selective right and left liver arteriograms, showing gastrointestinal vascular anatomy and flow characteristics.
When the branch of the hepatic artery supplying the tumor is identified the catheter is selectively placed within the artery, and the 90Y or 166Ho microspheres are infused.
Radiation dose absorbed, depends on microsphere distribution within the tumor vascularization.
Equal distribution is necessary to ensure tumor cells are not spared due to ~2.5mm mean tissue penetration.
The maximum penetration up to 11mm for 90Y or 8.7mm for 166Ho.
After treatment, for 90Y microspheres, SPECT or PET scanning may be done within 24 hours after radioembolization to evaluate the distribution.
Weeks after treatment, computed tomography or MRI can be done to evaluate anatomic changes.
Complications include postradioembolization syndrome, hepatic complications, biliary complications, portal hypertension and lymphopenia.
Complications due to extrahepatic deposition include radiation pneumonitis, gastrointestinal ulcers and vascular injury.
Postradioembolization syndrome (PRS) includes fatigue, nausea, vomiting, abdominal discomfort, and cachexia, occurring in 20-70% of patients.
Steroids and antiemetic agents may decrease the incidence of postradioembolization syndrome .
Liver complications include cirrhosis leading to portal hypertension, radioembolization-induced liver disease, transient elevations in liver enzymes, and fulminant liver failure.
Radioembolization-induced liver disease, is characterized by jaundice, ascites, hyperbilirubinemia and hypoalbuminemia developing at least 2 weeks-4 months after SIRT, absent tumor progression or biliary obstruction.
It is related to exposure of healthy liver tissue to radiation.
RCTs have shown safety and efficacy of 90Y therapy for the treatment of both primary and metastatic liver malignancies.
Treatment with radioablation with ytrium-90 In patients with metastatic colorectal cancer median survival of 11.6 months in the above study.
In a phase 2 clinical trial, radioembolization resulted in a 43% objective response rate in patients with metastatic liver neuroendocrine neoplasms previously given peptide radionuclide therapy.
The study investigated the safety and efficacy of additional holmium-166 (166Ho) radioembolisation after peptide receptor radionuclide therapy in patients with metastatic liver neuroendocrine neoplasms
Findings showed that 14 (43%) patients had an objective response in the treated liver volume.
Abdominal pain, increased y-glutamyl transpeptidase, and lymphocytopenia were the most common grade 3-4 adverse events, and were deemed manageable.
Radioembolization can be considered in patients with bulky liver disease, including after peptide receptor radionuclide therapy.
