 Pylorus-preserving pancreaticoduodenectomy (PPPD) is indicated for the following benign conditions:
Pylorus-preserving pancreaticoduodenectomy (PPPD) is indicated for the following benign conditions:
Benign periampullary neoplasms not amenable to local resection with ampullectomy
Benign duodenal neoplasms not amenable to local resection
Pancreatoduodenal trauma
PPPD is also indicated for the following malignant conditions:
Pancreatic ductal adenocarcinoma (PDAC)
Ampullary carcinoma
Distal CBD carcinoma (cholangiocarcinoma)
Duodenal carcinoma
Pancreatic islet cell carcinoma
Malignant intraductal papillary-mucinous neoplasm (IPMN) and mucinous cystic neoplasm (MCN)
Resectability is best described as the absence of contraindications for resection.
The pancreas is prismoid in shape and appears triangular in cut section, with superior, inferior, and anterior borders as well as anterosuperior, anteroinferior, and posterior surfaces.
The head of the pancreas lies in the duodenal C loop in front of the inferior vena cava (IVC) and the left renal vein.
The uncinate process is an extension of the lower half of the head toward the left; it is of varying size and is wedged between the superior mesenteric vessels in front and the aorta behind it.
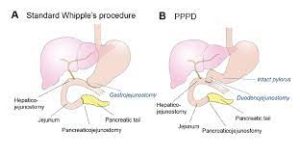
The comparison between the classically described pancreaticoduodenectomy and PPPD has not detected any significant differences with regard to operating time, perioperative morbidity, perioperative mortality, and long-term survival at 1, 3, and 5 years.
Thus, PPPD is a a technical variant of pancreaticoduodenectomy, in which blood supply to the proximal duodenum is preserved.
PPPD is not be performed with large, bulky tumors or with any tumor that may involve the first or second portion of the duodenum.
With the gastric antrectomy performed in classic pancreaticoduodenectomy an average of four more nodes are harvested with than would be harvested with PPPD: these will be positive for nodal metastases approximately 5% of the time.
Patients who undergo PPPD have a much higher incidence of delayed gastric emptying than those who undergo classic pancreaticoduodenectomy.
Delayed gastric emptying is the primary morbidity with PPPD.
The lack of statistical difference between classic pancreaticoduodenectomy and PPPD with regard to patient morbidity, mortality, and survival, the surgeon’s choice of approach should be based on the individual patient profile and the specific characteristics of the tumor.
A pancreatic-protocol contrast-enhanced CT with thin collimation is the most effective tool for identifying local extension.
The tumor can be evaluated in relation to important vascular structures.
A fat plane should be seen between the low-density tumor and surrounding structures.
The disease is considered resectable if the following conditions are met:
The tumor does not encase the celiac axis or Superior mesenteric artery and does not involve >180º of circumference.
The superior mesenteric vein (SMV), the portal vein (PV), and the SMV-PV confluence are all patent, with no thrombosis.
There is no extraregional nodal disease
There is no distant metastatic disease
Comparing classic Whipple pancreaticoduodenectomy with PPPD in a total of 465 patients with periampullary or pancreatic carcinoma.:There is no significant differences in mortality, morbidity, or survival between the two operations.
Some perioperative outcome measures favored PPPD to a significant degree.
Duodenal transection if PPPD permissible
Bulky neoplasms of the pancreatic head, tumors progressing to the first or second part of the duodenum, or clinically positive regional lymph nodes noted at this juncture preclude pylorus preservation.
The duodenum is transected 2-3 cm distal to the pylorus.
A two-layer end-to-side pancreaticojejunostomy, also known as a duct-to-mucosa reconstruction, is performed.
Hepaticojejunostomy is performed as a one-layer end-to-side anastomosis between the CHD remnant and a site on the jejunum distal to the pancreaticojejunal anastomosis.
Pancreatic leak may occur and lead to pancreatic fluid collection, pancreatic fistula formation, intra-abdominal abscess, or sepsis.
Possible long-term morbidity of PPPD:
Recurrence of malignancy, such as local recurrence at the retroperitoneal margin or distant recurrence in the liver, peritoneum, or lungs.
Pancreatic insufficiency – Exocrine (~40%), endocrine (~20%)
Pancreatic anastomotic stricture (recurrent pancreatitis, chronic pancreatic pain
Anastomotic failure
Anastomotic stricture
Small-bowel obstruction
Internal herniation of bowel
Small-bowel volvulus
