 In health plasma/serum potassium (K+) is maintained within the approximate reference range of 3.5 to 5.2 mmol/L, with serum values being slightly higher (∼ 0.4 mmol/L) than those of plasma because the process of blood clotting, essential to recovery of serum samples, is associated with release of potassium from activated platelets.
In health plasma/serum potassium (K+) is maintained within the approximate reference range of 3.5 to 5.2 mmol/L, with serum values being slightly higher (∼ 0.4 mmol/L) than those of plasma because the process of blood clotting, essential to recovery of serum samples, is associated with release of potassium from activated platelets.
Hyperkalemia is diagnosed if patient result exceeds the upper limit of the local reference range.
Severe hyperkalemia, usually defined as serum/plasma K+ >6.5-7.0 mmol/L is associated with risk of potentially fatal cardiac arrhythmia and warrants emergency clinical intervention.
Probably, the two most common causes of hyperkalemia are chronic kidney disease (CKD) and certain prescribed drugs, but there are many others and, in particular cases, the cause is often multifactorial.
Determining the cause is vital in assessment of a patient presenting with unexplained hyperkalemia.
This determination should include consideration of the possibility that the potassium result is spuriously raised, pseudohyperkalemia,
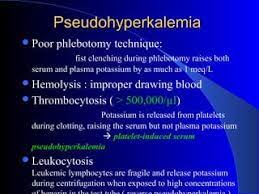
There are 2 broad causal aspects of pseudohyperkalemia: poor technique or practice during collection and preanalytic processing of samples; and pathological conditions that predispose to pseudohyperkalemia.
Potassium (K+) is the most abundant cation in the body and nearly all (∼98 %) of total body K+ (which amounts to approximately 3,500 mmol or 139 g) is contained within tissue cells.
Skeletal muscle is the most abundant tissue type, so skeletal muscle represents the largest reservoir of potassium in the body.
The intracellular fluid (ICF) potassium concentration of skeletal muscle cells is of the order of 100-150 mmol/L.
The remaining ∼2 % of total body potassium that is not contained within tissue cells is present in the extracellular fluid (ECF) at a concentration of just 4-5 mmol/L.
Cell membranes are permeable to ions such as K+.
The maintenance of the large concentration gradient across the cell membrane, essential for many cell functions, depends on the energy-consuming sodium-potassium pump (Na+-K+-ATPase) present in the membrane of all cell types.
This drives Na+ out of cells and K+ into cells, so whereas potassium is a predominantly intracellular cation, sodium is a predominantly extracellular cation
Blood plasma, which is that relatively small (approximate 25 %) portion of the total body ECF compartment that is contained within the vasculature, has a potassium concentration close to 5 mmol/L, and the three cell types that circulate suspended in blood plasma – erythrocytes, leukocytes and thrombocytes – have an ICF potassium concentration close to 100 mmol/L.
Since erythrocyte numbers far outstrip those of the other two blood cell types, erythrocytes represent by far the largest reservoir of K+ in blood.
The maintenance of the large differential between plasma and blood cell potassium concentration depends on the sodium-potassium pump (Na+-K+-ATPase) present in the membrane of blood cells.
The glycolytic pathway that ensures generation of energy-rich ATP from glucose is essential to the continuing function of the pump, so glucose can be considered the primary energy source that drives the pump.
The high concentration of potassium within blood cells relative to plasma concentration determines that a small release of potassium from blood cells can significantly increase plasma potassium concentration.
For this reason, the process of blood collection and handling preserves the physical and functional integrity of blood cell membranes until plasma or serum is separated from cells.
Many potential causes of pseudohyperkalemia can be explained in terms of in vitro reduction in blood cell membrane integrity or function and consequent in vitro release of potassium from blood cells to plasma or serum.
Pseudohyperkalemia is
Marked elevation of serum potassium (>0.4 mmol/L) compared to plasma potassium.
Familial pseudohyperkalemia, sometimes called leaky cell syndrome is a rare inherited presentation of pseudohyperkalemia.
is discussed in a little more detail below.
Causes of pseudohyperkalemia:
In vitro hemolysis
Fist clenching during phlebotomy
Undue delay in processing blood samples
Inappropriate storage temperature of blood samples
Potassium contamination of blood samples
In vitro hemolysis is the most common cause of pseudohyperkalemia.
Hemolysis is the lysis of erythrocytes with consequent release of their contents, including potassium and hemoglobin, to plasma.
In vivo hemolysis is a rare pathological feature of a number of diverse conditions and accounts for <2 % of all cases of hemolysis.
Any increase in plasma, or serum, potassium resulting from in vivo hemolysis is true hyperkalemia.
By contrast, in vitro hemolysis is a process that only occurs in blood removed from the body and is due to mechanical disruption of erythrocytes induced by the process of blood collection and handling.
Release of hemoglobin from erythrocytes during in vitro and in vivo hemolysis causes a color change in plasma and serum.
While plasma/serum is normally light straw colored but the presence of significantly increased amounts of hemoglobin turns it pinkish through to deep red, depending on the serum/plasma concentration of hemoglobin
Processes that can deleteriously impact on the integrity of erythrocytes and cause in vitro hemolysis:
Use of narrow-gauge needles
Use of syringe and needle rather than evacuated tube collection systems
Sampling blood via iv catheter
Non-standard, other than antecubital fossa, venipuncture site
Prolonged use of tourniquet
Vigorous shaking of samples after collection
Transportation of samples via some pneumatic tube transport systems (PTS)
Long-lasting /excessive centrifugation
The clenching of the fist in order to make veins more prominent, is associated with risk of pseudohyperkalemia: release of potassium from forearm muscle cells to surrounding interstitial fluid consequent on repeated or prolonged fist clenching.
Undue delay in processing blood samples is a potential cause of pseudohyperkalemia because the maintenance of in vivo potassium concentration depends on continuing activity of the sodium-potassium pump (Na+-K+-ATPase).
When blood is removed from the body, it cools towards room temperature,and that reduces activity of the glucose-metabolizing enzymes that generate ATP necessary for sodium-potassium pump function.
With the fall in temperature, the activity of the pump decreases with consequent efflux of potassium from blood cells to plasma/serum.
When all the glucose in the blood at the time of sampling is consumed and ATP can no longer be generated, the pump fails and potassium diffuses passively out of blood cells.
The plasma or serum should be separated from cells by centrifugation as soon as possible after blood is collected, and certainly within 3-4 hours of collection.
There is an inevitable delay in recovering serum samples because of the time-dependent (0.5 hour) process of clot retraction, so serum samples are potentially more prone to pseudohyperkalemia due to time delay than plasma samples.
Inappropriate storage temperature of blood samples during the time between collection and separation of serum or plasma from blood cells is a potential cause of pseudohyperkalemia.
Freezing whole-blood samples causes massive in vitro hemolysis and thereby severe pseudohyperkalemia.
The tendency to pseudohyperkalemia is greater for samples stored in a fridge at 4 °C than for samples stored at ambient room temperature ∼20 °C.
It is recommended that blood be stored at ambient temperature (15-25 °C) during the time between blood collection and separation of serum or plasma.
Pseudohyperkalemia is more frequent in winter months when ambient transport temperature is low (3-12 °C) than in summer months, when ambient transport temperature is higher (18-25 °C).
Allowing serum or plasma to be separated from cells before transport, eliminates seasonal pseudohyperkalemia.
Potassium contamination of blood samples is a potential cause of pseudohyperkalemia: most common contaminant is the potassium salt of ethylenediaminetetraaceticacid (K+EDTA), an anticoagulant additive present in tubes used to collect blood destined for hematological testing (FBC, CBC).
Blood samples may become contaminated with potassium if blood is sampled from the same arm that is being used to administer potassium-containing iv infusion.
The three pathological conditions that predispose to pseudohyperkalemia:
Inherited defects in erythrocyte membrane structure
Marked increase in platelet count (thrombocytosis)
Marked increase in white cell count (leukocytosis)
Two inherited defects in erythrocyte membrane structure predispose to pseudohyperkalemia; they are familial pseudohyperkalemia and dehydrated hereditary stomatocytosis.
Familial pseudohyperkalemia results from inheritance of mutation in the gene that codes for the erythrocyte membrane protein, ABCB6.
Its of inheritance is autosomal dominant and several mutations have been described, one of which is quite common, and present in 0.3 % of blood donors tested.
The genetic anomaly that defines FP causes increased in vitro leak of potassium from erythrocytes to plasma/serum when blood is exposed to temperatures below normal body temperature.
Affected individuals are asymptomatic and suffer no known deleterious effects as a result of FP, apart from this risk of pseudohyperkalemia.
Hereditary stomatosocytosis is an inherited mutation in the gene (PIEZO1) that codes for the erythrocyte membrane protein, PIEZ01, and
inherited as an autosomal dominant trait.
Thrombocytosis was the first identified cause of pseudohyperkalemia, due to increased in vitro release of potassium from activated platelets during the process of clotting and is therefore only a problem if serum is used to measure potassium.
Plasma potassium is unaffected by marked increase in platelet numbers.
Data suggests that serum potassium is falsely increased by 0.05 mmol/L for every 100×109/L increase in platelet count.
Individual with platelet count in excess of 500×109/L should have their potassium status assessed using plasma recovered from an anticoagulated blood sample or, alternatively, an anticoagulated whole-blood sample.
Extreme leukocytosis associated with hematological malignant disease can occasionally cause pseudohyperkalemia: most notably in patients with chronic lymphocytic leukemia (CLL) and very high white cells counts (>150×109/L).
Reverse pseudohyperkalemia occurs when plasma potassium is raised, and serum potassium normal, as in CLL with very high white dell counts, 120×109/L.
The mechanism of pseudohyperkalemia in the context of extreme leukocytosis is presumed to be in vitro white cell lysis and consequent efflux of potassium from white cells.
Studies implicate pneumatic tube transport systems (PTS) as the primary or contributory cause of extreme leukocytosis-related pseudohyperkalemia, suggesting fragile leukemic white cells are susceptible to lysis consequent to mechanical trauma.
There is a positive linear relationship between white blood count and the extent to which plasma potassium is spuriously increased: plasma potassium is spuriously increased by 0.6 mmol/L for every 100 x109/L increase in white blood count.
Signs and symptoms evident in those with severe hyperkalemia include:
characteristic ECG changes of peaked T waves
generalized weakness; muscle weakness/muscle cramps; and paresthesia
severe hyperkalemia can cause global paralysis.
Absence of signs and symptoms, along with no evidence of renal dysfunction should raise suspicion of pseudohyperkalemia.
A marked increase in platelet count (>500×109/L) or white cell count (>50×109/L) can cause pseudohyperkalemia.
