 Pouchitis refers to the inflammation of the ileal pouch, an artificial rectum surgically created out of ileum in patients who have undergone a proctocolectomy or total colectomy.
Pouchitis refers to the inflammation of the ileal pouch, an artificial rectum surgically created out of ileum in patients who have undergone a proctocolectomy or total colectomy.
The ileal pouch-anal anastomosis is created in the management of patients with ulcerative colitis, indeterminate colitis, familial adenomatous polyposis, cancer, or rarely, other colitides.
Pouchitis can occur in people who have had a colectomy or ileal pouch-anal anastomosis surgery to treat ulcerative colitis.
The incidence of a first episode of pouchitis at 1, 5 and 10 years post-operatively is 15%, 33% and 45% respectively.
The surgery involves removing part or all of the colon and creating a pouch from the end of the small intestine, which is then connected to the anus to allow for bowel movements.
Inflammation can develop in the pouch, which is called pouchitis.
It can cause symptoms such as abdominal pain, diarrhea, urgency, and fever.
Symptoms of pouchitis include increased stool frequency, urgency, incontinence, nocturnal seepage, abdominal cramping, pelvic discomfort, arthralgia, and impaired quality of life.
The exact cause of pouchitis is unknown.
Mechanisms can be the cause of pouchitis including: inflammatory factors such as a disbiosis sparked inflammation or Crohn’s disease of the pouch, surgical causes including surgical join leaks and pelvic sepsis, or infectious from Clostridium difficile (C Diff) or Cytomegalovirus (CMV).
It is possible to have more than one factor causing pouch inflammation at the same time.
Perhaps, it is related to an imbalance in gut bacteria or an impaired immune system response.
Approximately half a patient with ulcerative colitis, who undergo, restorative proctocolectomy with ileal pouch-anal anastomosis will subsequently, have pouchitis, and among those patients, 1/5 will have chronic pouchitis.
Treatment for pouchitis usually involves antibiotics and anti-inflammatory medications, and symptoms can improve with dietary changes, such as increasing fiber intake and avoiding certain foods.
Acute pouchitis is treated with short term antibiotic therapy.
Chronic pouchitis is defined by symptom duration longer than four weeks, occurs in approximately 1/5 of patients.
Tumor necrosis factor antagonists, vedolizumab, or ustekintumab may be effective in the treatment of pouchitis, that is refractory to antibiotics.
In severe cases, surgery may be required to remove the pouch.
Patients typically present with bloody diarrhea, urgency in passing stools, or discomfort while passing stools.
The loss of blood and/or dehydration resulting from the frequent stools will frequently result in nausea.
Extreme cramping and pain can occur with pouchitis.
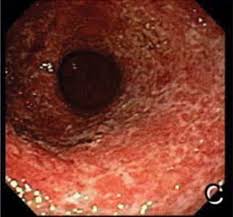
Endoscopy of the pouch (pouchoscopy) in patients with pouchitis usually reveals erythematous pouch mucosa, loss of pseudocolonic vasculature or other architecture, and friability of the mucosa. Biopsies show evidence of inflammatory cells or red blood cells in the lamina propria.
Symptom severity does not always correlate with severity of endoscopically or histologically evaluated pouch inflammation.
The most reliable tool for diagnosis is endoscopy combined with histologic features derived from tissue biopsies.
The duration of pouchitis is defined as acute (less than or equal to four weeks) or chronic (four weeks or more) and the pattern classified as infrequent (1–2 acute episodes), relapsing (three or fewer episodes) or continuous.
Finally, the response to medical treatment as labelled as treatment responsive or treatment refractory.
Treatment:
First line treatment is usually with antibiotics, specifically with ciprofloxacin and metronidazole.
Ampicillin or piperacillin can also be considered as alternatives to empiric ciprofloxacin and metronidazole.
Mettronidazole at a high daily dose of 20 mg/kg can cause symptomatic peripheral neuropathology in up to 85% of patients.
Other therapies which have been shown to be effective include probiotics.
Biologics, such as anti-tumor necrosis factor antibodies, may also be useful.
Treatment with vedolizumab is more effective than placebo in inducing remission in patients with chronic pouchitis, after undergoing ileal pouch, anal anastomosis for ulcerative colitis.
Vedolizumab is a gut selective monoclonal antibody approved for the treatment of moderately as severe, active ulcerative colitis, or Crohn’s disease in adults.
