
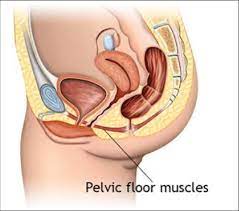

Pelvic floor physical therapy (PFPT) is focused on the rehabilitation of muscles in the pelvic floor after injury or dysfunction.
It can be used to address issues such as muscle weakness or tightness post childbirth, dyspareunia, vaginismus, vulvodynia, constipation, fecal or urinary incontinence, pelvic organ prolapse, and sexual dysfunction.
Pelvic floor physical therapy training addressesdysfunction in individuals across the gender and sex spectra, though PFPT is often associated with women’s health for its heavy focus on addressing issues of pelvic trauma after childbirth.
Therapists manually examine muscles of the pelvic floor both externally and internally, palpating to locate trigger points of pain and guide patients to manually tighten or loosen muscles to assess tone and function.
PFPT attempts to isolate the cause of dysfunction to one of two broader categories: low-tone or high-tone disorders.
Low-tone disorders, such as stress-urinary incontinence, overactive bladder, pelvic organ prolapse, and anal incontinence, are caused by weakened muscles in the pelvic floor.
High-tone disorders, such as pelvic floor myofascial pain, dyspareunia, vaginismus, and vulvodynia, are caused by overly strong or active muscles in the pelvic floor.
While low-tone disorders can be addressed through exercises such as Kegels meant to strengthen the pelvic floor, high-tone disorders can be worsened by such exercises and must be addressed through other means such as biofeedback or dilation training.
Pelvic floor disorders treated with PFPT
Chronic pelvic pain (CPP) dysfunctions of the pelvic region associated with long-term discomfort, and includes diagnoses such as dyspareunia, vaginismus, vulvodynia or vestibulodynia, endometriosis, interstitial cystitis, chronic nonbacterial prostatitis, chronic proctalgia, piriformis syndrome, hip dysfunction, and pudendal neuralgia.
Around 1 in 4 women and between 2% and 10% of men experience chronic pelvic pain, making CPP of high clinical relevance.
PFPT is considered to be a key element in the treatment of CPP, working to reduce pain or enhance function by normalizing pelvic floor muscle tone and endurance.
Many disorders that cause chronic pelvic pain,such as dyspareunia and vaginismus, are associated with discomfort during intercourse.
Treatment of CPP with pelvic floor physical therapy is often related to the treatment of sexual dysfunction.
With dyspareunia, patients often suffer from overactive pelvic floor muscles that are also weak in strength.
Pelvic floor physical therapy can help to both strengthen the PFMs as well as reduce the muscles’ resting muscle tone.
Pelvic floor physical therapy has also been shown to be effective in the treatment of erectile dysfunction (ED).
Pelvic floor physical therapy provides a treatment with less risk of complication than commonly prescribed medications or surgical interventions.
Randomized controlled trials have seen a range from modest to significant success with pelvic floor physical therapy treatments for ED.
PFPT has success in treating premature ejaculation.
It is possible that PFPT helps disorders such as ED and premature ejaculation simply because it enhances awareness and control over individual muscles or muscle groups in the pelvic region.
Passive muscular support and voluntary/reflexive contractions of the pelvic floor are important maintaining continence during bouts of increase in intra-abdominal pressure like and coughing, sneezing.
Stress incontinence can be treated with high success using PFPT.
The treatment of overactive bladder syndrome, and fecal incontinence with PFPT has shown more modest success.
Pelvic floor exercises focused on the pelvic floor muscles and core muscles which help to strengthen muscles to improve bladder control.
Benefits associated with pelvic floor physical therapy specifically in postpartum women including increasing muscle strength and endurance on top of decreasing the rate of urinary incontinence.
Higher than average pelvic floor physical tone may be a component of constipation, anismus, and irritable bowel syndrome.
Pregnancy and vaginal delivery have been proved to be the risk factors for the development of severe urinary incontinence as they could obviously weaken the pelvic floor muscle strength.
About 1/3 of women post-childbirth struggle with urinary incontinence,and women who attend PT can decrease the likelihood of developing urinary incontinence.
It is advisable to seek out a pelvic floor PT in the early stages of pregnancy.
Women after childbirth, regardless of the type of delivery are at high risk of new and prolonged signs of pre-existing signs of pelvic floor muscle dysfunction.’
Women who receive C-sections and who receive PT afterward improved pelvic floor muscle tone and strength and positively impact their daily function and sexual activity at 6 months postpartum.
