 Unpleasant sensory and emotional experience with actual or potential tissue damage.
Unpleasant sensory and emotional experience with actual or potential tissue damage.
In unpleasant sensory and emotional perception that is usually the result of underlying tissue pathology, but not always.
The interpretation of pain varies with the patient’s culture, language, prior experiences, the acuteness or chronic nature of pain and the very description of pain.
Paint affects the lives of millions of Americans and potentially reduces their level of function, mental health, and quality of life.
Pain history include: location, duration, exacerbating and relieving factors, and accompanying symptoms.
The transduction of pain involves conversion of mechanical, inflammatory or thermal stimuli into an electrical impulse.
Its function is to protect the body by making the individual aware of damaging events and to promote healing by causing sensitivity to movement or other stimuli that may delay recovery.
Pain, however, is not always related to tissue damage and does not always serve a protective function such as with neuropathic pain, fibromyalgia, and migraine.
These type of pain are caused by a lesion or disease of the somatosensory parts of the nervous system.
A defining feature of many illnesses.
Sensitivity to and sensation of pain are sex dependent, generally being heightened in female as compared with male subjects.
Studies have shown that sex hormones affect pain processing in humans.
Assessments of somatic sensation: pinprick pain sensitivity, incision-induced pain, and pinprick hyperalgesia, are significantly correlated with plasma P4 and follicle-stimulating hormone and negatively correlated with testosterone in humans.
Visceral pain is often regarded as more unpleasant, and it is more difficult to localize than somatic pain.
Visceral hypersensitivity consists of 2 components: allodynia, in which an innocuous stimulus is perceived as painful, and hyperalgesia, defined as a more intense perception of a painful stimulus.
The intensity and location of visceral pain is reflected by the somatosensory cortices of the lateral pain system.
Studies demonstrate that the biological basis for nociception difference between males and females in that microglia cells are critical modulators in neural networks in males whereas T cells are involved in females, with additional modulation provided by sex hormones.
Acute and chronic pain may cause suffering and interfere with daily activities of living, and influence the choice of treatment.
Approximately 11% of US adults report daily pain.
Can provide an index of disease severity and activitity of an underlying condition.
Often associated with poor general health, health-related disability, and increased health care utilization.
Acute pain is the most common reason for emergency department visits.
Surgical procedures are often associated with acute postoperative pain.
Chronic pain is one of the leading cause of years of lives with disability.
May be a prognostic indicator.
Requires consciousness to permit recognition of a stimulus as unpleasant.
Routinely undertreated, and pain care is often fragmented, without a comprehensive assessment or treatment plan.
While pain is commonly related to noxious stimuli, it is primarily a psychological construct that can exist in the absence of such stimuli, such as that seen with phantom limb pain.
The most common symptom reported in the general population and in primary care, and the leading cause of work disability and costs more than $600 billion each year in health care costs and lost productivity.
Approximately 126 million adult patients experience pain in a given year, and about one third or 40 million have severe pain.
The Institute of Medicine reports that acute and unspecified chronic pain affects 116 million Americans, approximately 30% of the general population.
CDC approximately 16% of men 22% of women have experienced pain in the last three months.
Men manage their pain through self-distraction and problem-focused challenges, whereas women resort to emotion-focused tactics, catastrophizing, positive self-statements, and social support.
Expression of pain is socially more acceptable among women, whereas men show increased pain tolerance and greater resistance in reporting pain.
Subjective complex experience perceived only by the patient with associated physical, psychological and cognitive aspects.
Back pain, joint pain, neck pain, and headaches are the most common types of pain in US adults.
Perception requires cortical recognition of stimuli as unpleasant.
Perception of pain involves two main groups of neural pathways ascending and descending.
Peripheral nerves transmit sensory signals, including pain inducing signals, to the spinal cord for transmission via the ascending nociceptive pathway to the brain for processing.
The transmission and perception of pain is modified by neuromodulators released from nonneuronal cells contributing to hyperalgesia and include mast cells.
Nociceptive signals from nociceptors in peripheral nerves are activated by stimuli such as temperature and physical pressure.
Perception of pain has a normal distribution on a bell curve.
Pain may be episodic, with many patients reporting symptoms that resolve and then recur with varying time periods in between
Descending pain pathways send both facilitatory and inhibitory signals from the brain to the spinal cord and to the periphery, either increasing or decreasing the volume of incoming nociceptive signals reaching the brain.
Neurotransmitters and neurochemicals mediate signals in neural pathways.
Pain causes alterations in the neurocircuitry related to reward, resulting in vulnerability to suicide and to riskier use of opioids.
Chronic pain is linked to suicide, and is associated with opioid overdose.
Sensory receptor afferents synapse on neurons in the spinal cord and their axons project to the thalamus which in turn ends afferents to the cerebral cortex.
In general health care professionals underestimate an individuals pain levels while family members tend to overestimate the same.
Assessment of the presence and degree of pain can be influenced by cognition, consciousness, cultural, ethnic and gender considerations.
Prevalence of pain in nursing home 45%-80%, with analgesics being used in 40% to 50% of residents.
25-50% of community adults report daily pain.
Two thirds of pain related outpatient visits are related to musculoskeletal pain, which accounts for nearly 70,000,000 outpatient visits in the US annually.
Overall pain prevalence of 46% in southern Sweeden, with prevalence increasing into the eigth decade up to 55% experiencing chronic pain (Jakobsson U).
85-90% of patients with cancer pain are well managed.
10-15% of patients with cancer will have pain that is resistant to traditional analgesic management.
41% of patients with cancer pain suffer from inadequate pain management.
About 4 million U.S. patients have cancer pain.
Generally divided into two categories: nociceptive and neuropathic.
Electronic impulses are generated within tissue nociceptors, responsible for conducting pain signals into the dorsal horn of the spinal cord.
Nociceptors found in the dorsal root ganglia transmit pain signals along A delta fibers which are myelinated axons, and C fibers which are unmyelinated axons.
Unmyelinated C-fiber nociceptors have a sensory afferent function transitting information about noxious stimulation to the CNS and serve efferent function causing vasodilation and plasma extravasation called neurogenic inflammation.
Activation of C-fibers causes action potentials to travel along the axon to the CNS and invade endings of their arborizations. leading to release of neuropeptides P and calcitonin gene related peptide producing neurogenic inflammation.
Nociceptive pain induced when nociceptive receptors are stimulated by tissue damage.
Nociceptive pain originates from healthy tissue nociceptors activated by local release of substances.
Nociceptive pain often responds to analgesics.
Nociceptive pain subdivided into visceral and somatic pain.
Bone pain is the most common type of nociceptive cancer pain
Somatic type is described as achy, throbbing or dull and is more easily localized than visceral pain.
Classified by: duration, cause, anatomic location, temporal characteristic, organ system, mechanism and syndrome.
Neuropathic pain induced by changes in the CNS and peripheral nervous systems with sharp, burning, tingling or electrical sensation.
Widespread chronic idiopathic pain affects approximately 10% of the population.
Acute pain often follows injury, structural degeneration, infection or metabolic alterations and usually abates associated tissues heal.
Chronic pain defined associated pain lasting more than 3-6 months or lasting one month longer than the usual time required for an injury the heal.
Pain increases an individual’s risk for developing insomnia.
BDNF is a short-term promoter, but a long-term inhibitor of pain sensitivity, as a result of its effect as inducer of neuronal differentiation.
Chronic musculoskeletal pain occurs in 5-20% of pediatric patients with approximately 7% of school-age children reporting pain symptoms lasting more than 3 months.
Visceral pain, from internal organs, is often poorly localized and characterized as squeezing, cramping or colicky if from a hollow viscus and described as aching or dull if from a solid organ.
Several organs are insensitive to pain until capsule or adjacent tissues become involved and include: liver, lungs, and kidneys.
Visceral pain can be diffuse, associated with cramping or gnawing sensations, can be referred to distant sites, making the isolation of the source of pain difficult.
The degree of pain does not correlate well with identifiable tissue injury.
WHO three step ladder approach to cancer pain successful in 77-100% when used appropriately.
Pain management is complicated by limited access to pain treatments and lack of clarity regarding the evidence supporting pain treatments.
Many individuals with pain cannot access the full range of potentially helpful therapies and there are disparities in pain management according to race, ethnic group, gender, socioeconomic status, and population density.
With mild pain step 1 nonopioid analgesics such as acetaminophen or nonsteroidal anti-inflammatory drugs are indicated.
WHO analgesic ladder: guidelines recommend a sequential three-step approach for analgesic administration based on pain severity-with non-opioids for mild pain, weak opioids for moderate pain, and strong opioids for severe pain.
In the above recommendations drug selection is based on the severity of the pain, to use oral medications whenever possible, to use a fixed scheduled dosing according to pharmacokinetics of the drug rather then on demand, and regular assessment and reevaluation of pain.
it is recommended drugs used in step 1 to be continued as opioids are added to provide an improved analgesic control with different mechanisms of action and reduce opioid requirements and adverse effects.
Opioids continue to be commonly used to treat pain, despite evidence that the short term benefits are small, and despite limited evidence of long-term benefits.
Pain contributed to functional decline in the elderly is associated muscle weakness, mobility limitations that could increase the risk of falls.
The Maintenance of Balance, Independent Living, Intellect, and Zest in the Elderly (MOBILIZE) study, a population based longitudinal study of falls involving 749 adults age 70 years or older: Patients with chronic pain at baseline are at greater risk for falls, and the greatest risk for falls were in those with 2 or more pain sites (Leveille SG).
Moderate pain treated with step 2 weak opioids in addition to step 1 medications.
Severe pain treated with step 3 strong opioids.
Tricyclic antidepressants are effective adjuvant treatments in managing headache and neuropathic pain.
Methadone and levophanol are potent mu-opioid agonists that inhibit thereuptake of norepinephrine and block N- methyl-D-aspartate receptors in the CNS, which typically improves efficacy specifically for neuropathic bases pain aymptoms.
Untreated pain in the short term results in higher energy expenditure and immunomodulation.
Longer-term untreated pain increases the risk of posttraumatic stress disorder.
Management of pain requires appropriate assessment with documentation of pain characteristics, understanding the mechanisms of pain, identifying modulating factors and reassessments over time.
It is necessary to characterize pain by intensity, location, medical treatments, frequency, onset, position, quality, radiation of pain, severity, and triggers which can provide diagnostic clues to the mechanism of pain.
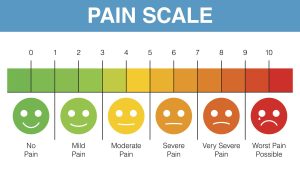
Pain intensity is the standard for pain assessment.
The most commonly used scales for pain assessmenton the numeric rating scale 0-10, with 0, no pain and 10, worst possible pain, no visual analog scale 0-100 mm with 0, no pain and 100 worse possible pain, and the categorical scale none, mild, moderate, and severe.
Generally, a numeric score of 1-3, 4-6, and 7-10 corresponds to mild, moderate, and severe pain, respectively.
Pain intensity assessment should be a routine screening process and serially monitored.
Pain characteristics can provide diagnostic clues to underlying etiology.
Somatic nociceptive pain such as from bone metastases, wounds or mucositis will be described as achy, stabbing, throbbing, squeezing, tender, and or deep and is site-specific.
Visceral nociceptive pain such as from liver metastases, bowel obstruction, coronary ischemia, urinary retention will be described as sharp, stabbing, squeezing, crampy, and or gnawing with vague and difficult to locate pain which may be referred in nature.
Neuropathic pain that may be related to spinal cord compression, radiculopathy, peripheral neuropathy, phantom limb, postmastectomy, thoracotomy pain may be described as burning, shooting, tingling, numbness, scalding and may be associated with allodynia and/or hyperalgesia with radiation along nerve distribution.
Many common pain conditions such as neuropathic pain, including diabetic neuropathic pain and postherpetic neuralgia, respond better to non-opioids, such as antiepileptics and serotonin-norepinephrine reuptake inhibitors.
For conditions like fibromyalgia, opioids provide little benefit.
While the number of prescriptions for opioids continues to climb there is not a commensurate improvement in the care of patients with pain.
Prescribing both benzodiazepines and opioids for pain is generally not beneficial, and increase toxicity and are bothcommonly involved in unintentional drug overdoses.
In almost 30% of opioid overdose deaths, a benzodiazepine is also involved.
Benzodiazepines can interfere with the analgesic effects of opioids and leading to a need for increased doses of opioids to get the same analgesic effect.
Prolonged use of benzodiazepines can lead to hyperalgesia.
Pain in children and adolescents can be predictive of pain in adulthood.
Most common pains in children and adolescents involve the low back, head, and abdomen.
