Organ transplantation: medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ.
Organs and/or tissues that are transplanted within the same person’s body are called autografts.
Transplants that are recently performed between two subjects of the same species are called allografts.
Allografts can either be from a living or cadaveric source.
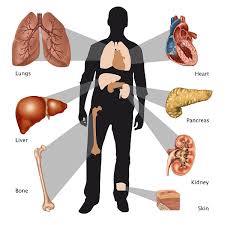
Organs that have been successfully transplanted include the heart, kidneys, liver, lungs, pancreas, intestine, thymus and uterus.
Tissues include bones, tendons, corneae, skin, heart valves, nerves and veins.
Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart.
Cornea and musculoskeletal grafts are the most commonly transplanted tissues.
Cornea and musculoskeletal grafts outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death.
Tissue may be recovered from donors who die of circulatory death, as well as of brain death, for up to 24 hours past the cessation of heartbeat.
Most tissues with the exception of corneas, and unlike organs can be preserved and stored for up to five years.
Transplantation bioethical issues include: the definition of death, when and how consent should be given for an organ to be transplanted, payment for organs for transplantation, transplantation tourism, the socio-economic context in which organ procurement or transplantation may occur, organ trafficking, and the ethical issue of not holding out false hope to patients.
A key area for medical management is transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient.
Transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
Autografts are the transplant of tissue to the same person.
Autografts can be done with surplus tissue, tissue that can regenerate, or tissues needed more elsewhere: skin grafts, vein extraction for CABG.
Some autografts are done to remove the tissue and then treat it or the person before returning it: include stem cell autograft and storing blood in advance of surgery.
An allograft is a transplant of an organ or tissue between two genetically non-identical members of the same species.
Most human tissue and organ transplants are allografts.
The genetic difference between the organ and the recipient, results in the recipient’s immune system recognizes the organ as foreign and attempts to destroy it, causing transplant rejection.
The risk of transplant rejection can be estimated by measuring the panel-reactive antibody level.
An isograft is a subset of allograft in which organs or tissues are transplanted from a donor to a genetically identical recipient, such as an identical twin.
Isografts do not trigger an immune response.
A xenograft is a transplant of organs or tissue from one species to another:
porcine heart valve transplant.
Xenotransplantation is often an extremely dangerous type of transplant because of the increased risk of non-functional compatibility, rejection, and disease carried in the tissue.
Very young children, under 12 months, but often as old as 24 months do not have a well-developed immune system, and it is possible for them to receive organs from otherwise incompatible donors.
Graft survival and children’s mortality are approximately the same between ABOi and ABO-compatible (ABOc) recipients.
The most important factors in graft survival are that the recipient not have produced isohemagglutinins, and that they have low levels of T cell-independent antigens.
Regulations allow for ABOi transplantation in children under two years of age if isohemagglutinin titers are 1:4 or below,and if there is no matching ABOc recipient.
Limited success has been achieved in ABO-incompatible heart transplants in adults, with recipients that have low levels of anti-A or anti-B antibodies.
Renal transplantation is more successful, with similar long-term graft survival rates to ABOc transplants.
Types of donor
Organ donors may be living or may have died of brain death or circulatory death.
Most deceased donors are those who have been pronounced brain dead.
Brain dead means the cessation of brain function, typically after receiving an injury to the brain, or otherwise cutting off blood circulation to the brain.
Breathing is maintained via artificial sources, which, in turn, maintains heartbeat.
Once brain death has been declared, the person can be considered for organ donation.
Because less than 3% of all deaths in the US are the result of brain death, the overwhelming majority of deaths are ineligible for organ donation, resulting in severe shortages.
Organ donation is possible after cardiac death in some situations, primarily when the person is severely brain-injured and not expected to survive without artificial breathing and mechanical support. Independent of any decision to donate, a person’s next-of-kin may decide to end artificial support.
If the person is expected to expire within a short period of time after support is withdrawn, it allows quick recovery of the organs after circulatory death has occurred.
Tissues may be recovered from donors who die of either brain or circulatory death.
Tissues may be recovered from donors up to 24 hours past the cessation of heartbeat.
In contrast to organs, most tissues, with the exception of corneas, can be preserved and stored for up to five years.
More than 60 grafts may be obtained from a single tissue donor.
Because of the ability to recover from a non-heart-beating donor bank tissue, the number of grafts available from each donor – tissue transplants are much more common than organ transplants.
More than one million tissue transplants take place in the United States each year.
Tissue transplants include: cornea, bone, tendon, skin, pancreas islets, heart valves, nerves and veins, cells – bone marrow and stem cells.
In living donors, the donor remains alive and donates a renewable tissue, cell, or fluid such as blood, or skin, or donates an organ or part of an organ in which the remaining organ can regenerate or take on the workload of the rest of the organ (kidney donation, partial donation of liver, lung lobe, small bowel).
Deceased donors are declared brain-dead and their organs are kept viable by ventilators or other mechanical mechanisms until they can be excised for transplantation.
Apart from brainstem-dead donors, who have formed the majority of deceased donors for the last 20 years, there is increasing use of after-circulatory-death donors to increase the potential pool of donors as demand for transplants continues to grow.
Prior to the legal recognition of brain death in the 1980s, all deceased organ donors had died of circulatory death.
These organs have inferior outcomes to organs from a brain-dead donor.
Patients who underwent liver transplantation using donation-after-circulatory-death allografts have been shown to have significantly lower graft survival than those from donation-after-brain-death allografts due to biliary complications and primary nonfunction in liver transplantation.
Countries often have formal systems in place to manage the process of determining who is an organ donor and in what order organ recipients receive available organs.
The overwhelming majority of deceased-donor organs in the United States are allocated to the Organ Procurement and Transplantation Network, by the United Network for Organ Sharing, or UNOS.
UNOS does not handle donor cornea tissue; corneal donor tissue is usually handled by various eye banks.
Liver allocation is based partially on MELD score.
Directed or targeted donation, occurs when the family of a deceased donor requests an organ be given to a specific person, subverts the allocation system.
A “paired-exchange” is a technique of matching willing living donors to compatible recipients using serotyping.
One may be willing to donate a kidney to their partner/friend but cannot since there is not a biological match.
The willing donor is a a match to a different recipient who also has an incompatible but willing donor.
The second donor must match the first recipient to complete the pair exchange.
Paired-donor exchange, may more efficiently allocate organs and lead to more transplants.
Good Samaritan or altruistic donation refers to giving a donation to someone that has no prior affiliation with the donor.
In compensated donation, common in some parts of the world , donors get money or other compensation in exchange for their organs.
Compensated donation is one of the many factors driving medical tourism.
Hypothermic perfusion for transplantation of kidneys and liver and normothermic perfusion has been used effectively in the heart, lung, liver and, less so, in the kidney.
