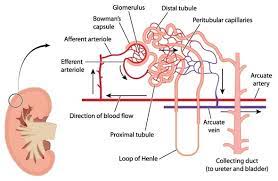
In the kidney, the loop of Henle is the portion of a nephron that leads from the proximal convoluted tubule to the distal convoluted tubule.
The loop of Henle’s main function is to create a concentration gradient in the medulla of the kidney.
Its countercurrent multiplier system, using electrolyte pumps, creates an area of high urea concentration deep in the medulla, near the papillary duct in the collecting duct system.
Water present in the filtrate in the papillary duct flows through aquaporin channels out of the duct, moving passively down its concentration gradient, reabsorbing water and creating a concentrated urine for excretion.
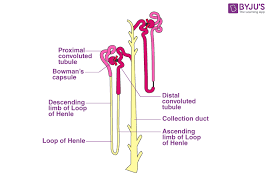
The loop of Henle can be divided into four parts:
Thin descending limb of loop of Henle, which has low permeability to ions and urea while being highly permeable to water.
The loop has a sharp bend in the renal medulla going from descending to ascending thin limb.
The thin ascending limb is impermeable to water, but it is permeable to ions.
Ascending limb of loop of Henle
Sodium (Na+), potassium (K+) and chloride (Cl−) ions are reabsorbed from the urine by secondary active transport by a Na–K–Cl cotransporter (NKCC2).
The electrical and concentration gradient drives more reabsorption of Na+, as well as other cations such as magnesium (Mg2+) and calcium (Ca2+).
The cortical thick ascending limb drains urine into the distal convoluted tubule.
The tissue of the loop is squamous epithelium, and the thick and thin terminology refers to the size of the epithelial cells.
The loop of Henle is supplied by blood by capillaries descending from the cortical efferent arterioles, the vasa recta.
The vasa recta have a countercurrent multiplier mechanism that prevents washout of solutes from the medulla, thereby maintaining the medullary concentration.
Water is osmotically driven from the descending limb into the interstitium, and readily enters the capillaries.
The low bloodflow through the vasa recta allows time for osmotic equilibration.
Blood in the vasa recta has large proteins and ions which were not filtered through the glomerulus. providing an oncotic pressure for ions to enter the vasa recta from the interstitium.
The main function of the loop of Henle is to set up a concentration gradient.
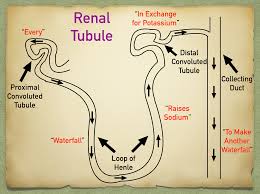
The descending loop of Henle receives isotonic (300 mOsm/L) fluid from the proximal convoluted tubule (PCT).
The PCT fluid is isotonic because as ions are reabsorbed by the gradient system, water is also reabsorbed maintaining the osmolarity of the fluid.
Substances reabsorbed in the PCT include urea, water, potassium, sodium, chloride, glucose, amino acids, lactate, phosphate, and bicarbonate.
As water is also reabsorbed the volume of fluid in the loop of Henle is less than the PCT, approximately one-third of the original volume.
The interstitium of the kidney increases in osmolarity outside as the loop of Henle descending from 600 mOsm/L in the outer medulla of the kidney to 1200 mOsm/L in the inner medulla.
The descending portion of the loop of Henle is very permeable to water and is less permeable to ions.
Water is easily reabsorbed in the descending loop of Henle and solutes are not readily reabsorbed.
The 300 mOsm/L fluid from the loop loses water to the higher concentration outside the loop and increases in tonicity until it reaches its maximum at the bottom of the loop.
The descending loop represents the highest concentration in the nephron, but the collecting duct can reach this same tonicity with maximum ADH effect.
The ascending limb of the loop of Henle receives an even lower volume of fluid and has different characteristics compared to the descending limb.
In the ascending portion, the loop becomes impermeable to water and the cells of the loop actively reabsorb solutes from the luminal fluid;
In the ascending portion of the loop water is not reabsorbed and ions are readily reabsorbed.
As ions leave the lumen via the Na–K–Cl symporter and the Na–H antiporter, the concentration becomes more and more hypotonic until it reaches approximately 100–150 mOsm/L.
The ascending limb is also called the diluting segment of the nephron because of its ability to dilute the fluid in the loop from 1200 mOsm/L to 100 mOsm/L.
Flow of the fluid through the entire loop of Henle is slow.
As flow increases, the ability of the loop to maintain its osmolar gradient is reduced.
The vasa recta have a slow flow as well.
Increases in vasa recta flow wash away metabolites and cause the medulla to lose osmolarity as well.
Increases in flow will disrupt the kidney’s ability to form concentrated urine.
The loop of Henle reabsorbs around 25% of filtered ions and 20% of the filtered water in a normal kidney.
These ions are mostly Na+, Cl−, K+, Ca2+ and HCO3−.
The length of the loop of Henle limits the concentration of the gradient.
The longer the loop, the greater the osmotic gradient, and the greater capacity to concentrate urine.
Through the countercurrent multiplier the loop of Henle increases the osmolarity of the medulla.
The loop of Henle is always a U-shaped tubule with an descending limb and an ascending limb.
The loop of Henle has two functions; the first is to clean wastes, the second is to maintain a balance between ions and H2O,
allows it to balance the blood pressure, blood pH and membrane potentials.
The loop of Henle coordinates its function with the collecting duct to regulate the amount of water to reabsorb or to excrete.
The loop of Henle makes the medulla of the kidney salty, the collecting duct regulates the permeability of water that could be reabsorbed to such salty environment.
The saltier the medulla, the more water can be reabsorbed from the pre-urine in collecting duct; before it becomes urine.
Aquaporin-2 (AQ2) sits in collecting duct and is selectively inserted into cell membranes, according to the body’s needs, to reabsorb water to create that balance.
The urine concentration in humans can be as concentrated as 1400 mOsm which is limited by the length of our loop of Henle-2.2 mm.
