 The myeloblast is a unipotent stem cell which differentiates into the effectors of the granulocyte series.
The myeloblast is a unipotent stem cell which differentiates into the effectors of the granulocyte series.
It is found in the bone marrow.
G-CSF stimulates myeloblasts and other cytokines triggers maturation, differentiation, proliferation and cell survival.
Myeloblasts reside extravascularly in the bone marrow.
Hematopoiesis takes place in the extravascular cavities between the sinuses of the marrow.
The hemopoietic cells are aligned in cords or wedges between these sinuses, with myeloblasts and other granular progenitors concentrated in the subcortical regions of these hemopoietic cords.
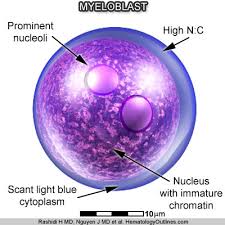
Myeloblasts are small cells with a diameter between 14 and 18μm.
It has a large oval nucleus composed of very fine nonaggregated chromatin and possessing 3 or more nucleoli.
The cytoplasm has a basophilic character.
It is devoid of granules, which is a major difference from the promyelocyte.
The nucleolus is the site of assembly of ribosomal proteins, which are located in various particles dispersed over the cytoplasm.
Mitochondria are present but have a small size.
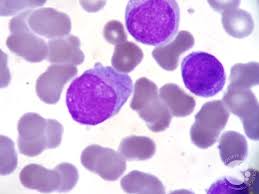
Distinguish a myeloblast from a lymphoblast upon microscopic examination- the presence of cytoplasmic granules, the lesser degree of condensation in the nuclear chromatin, and the increased prominence of the nucleoli.
Myeloblast cells descend from the primitive reticulum cells, which are found in the stroma of the marrow.
The primitive reticulum cells, namely the hemocytoblast, develop into blood cell lines like erythropoiesis and thrombopoiesis.
Granulopoiesis is regulated by humoral agents, like colony-stimulating factor (CSF) and interleukin 3.
Granulopoiesis consists of 5 stages, in which the myeloblast is the first recognizable cell.
Next in the differentiation sequence is the monoblast and the promyelocyte, which can develop into one of three different precursor cells: the neutrophilic, basophilic or eosinophilic myelocyte.
This proliferation takes five divisions before the final stage is obtained.
With malfunctioning myeloblasts in acute myeloblastic leukemia, the main clinical features are caused by failure of hemopoiesis with anemia, hemorrhage and infection.
There is a progressive accumulation of these leukemic cells, because some blast progenitor cells renew themselves and have a limited differentiated division.
Myeloblasts are immature leukocytes that arise from progenitor stem cells in the bone marrow, and their presence in the peripheral blood suggest a pertubation of normal hematopoetic differentiation.
Myeloblasts are characterized by the presence of CD34 and CD117 antigens, identified with flow cytometry.
A peripheral blood myeloblasts count of greater than 20% is diagnostic of acute myelogenous leukemia.
Causes of elevated peripheral blood myeloblasts with leukocytosis include AML, myelodysplastic syndrome, myeloproliferative neoplasms, severe infection, bone marrow damage, or infiltration by fibrosis, malignancy or infection, and administration of G-CSF.
