 An opportunistic infection caused by species of Mycobacterium that can cause severe illness in people with advanced AIDS but rarely affects others.
An opportunistic infection caused by species of Mycobacterium that can cause severe illness in people with advanced AIDS but rarely affects others.
An indolent nontuberculosis mycobacterial (NTM) lung disease.
MAC frequently colonizes the airway and rarely results in infection in healthy and immunocompete persons.
M. avium and M intracellulare are the two different species of mycobacteria implicated.
The 2 agents are difficult to differentiate and the combined name of MAI is used.
The risk of disseminated MAC disease is directly related to the severity of immunosuppression.
Typically occurs in persons with CD4 counts of <50 cells/µL, and its frequency increases as the CD4 count declines.
Immunocompromised patients and those with structural lung disease, such as bronchiectasis, are at risk of the development of a MAC pulmonary disease.
In most cases the source of infection is environmental, such as soil, milk, dust, and home water systems.
Household water, hot tubs and shower head are frequent reservoirs.
Can occur in up to 40% of AIDS patients with CD4 counts of <50 cells/µL.
On average takes 25 weeks to establish the diagnosis.
MAI lung disease can occur in otherwise healthy patients.
The presence of non-tuberculosis mycobacterium in sputum does not equate to disease.
Diagnosis requires a combination of clinical, imaging, and microbiologic findings and M. Tuberculosis must be ruled out.
Skin testing and interferon-gamma release assays have no diagnostic role but are indicated to exclude M. Tuberculosis if clinical suspicion is high.
If either diagnosis, tuberculosis or pulmonary nontuberculosis mycobacterium infection is suspected in sputum cultures are equivocal, then isolation precautions should be followed.
Patients may present with fevers, night sweats, weight loss, anorexia, chronic diarrhea, fatigue, weakness, and abdominal pain.
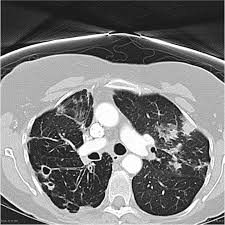
Diagnosis includes respiratory symptoms with presence of abnormal lung CT findings, exclusion of other causes of symptoms, and microbiologic data supporting the diagnosis.
Microbiological diagnosis includes isolation from three separate adequate sputum samples or one bronchoscopic or lung biopsy sample.
Diagnosis requires isolation of MAC from the blood or other normally sterile body fluids or tissues and M avium cultured from sputum, bronchial washing, or stool may represent colonization rather than infection.
Patients complain of progressive, paroxysmal cough with variable sputum production punctuated by exacerbation.
Predisposing conditions include suppressed cough reflex, poor mucociliary clearance, and chronic obstructive pulmonary disease.
Other risk factors include GERD, low body mass index, thoracic skeletal abnormalities, treatment with antitumor necrosis factor-alpha agents and corticosteroid use.
May take weeks to grow in culture.
If blood cultures are negative, consider biopsy of the lymph nodes, bone marrow, liver, bronchoscopy, or bowel to detect MAC by microscopic examination for AFB and culture.
Antimicrobial resistance develops quickly with single-drug therapy, therefore multidrug regimens must be administered.
Three clinical syndrome presentations are typical: 1)Men with a history of smoking or previous lung disease with fibrocavitary lesions in the upper lobe on CT scan, 2)nodular bronchiectasis encompassing a subset of tall, gaunt, non-smoking elderly women with bronchiectasis of the right middle lobe or lingula, with habitual cough suppression, leading to infection of poorly draining areas of the lung that depend length on voluntary expectoration, 3) the least common form is hypersensitivity pneumonitis, known as hot-tub lung. An acute reaction triggered by inhalation of bacteria containing mist from the surface of hot tubs, baths, pools, and metalworking fluids.
Therapy is determined on a case-by-case basis.
Antimicrobial regimens, which usually incorporate a macrolide antibiotic, are based on species and clinical severity.
In vitro sensitivities to M. avium to antimycobacterial agents are of no utility because of poor correlation with clinical response.
It is recommended that susceptibility testing for M. avian complex limited to macrolides.
Treatment regimens recommended by the U.S. Centers for Disease Control and Prevention include 2-drug regimens: Clarithromycin 500 mg twice daily + ethambutol 15 mg/kg once daily or Azithromycin 500-600 mg once daily + ethambutol 15 mg/kg once daily.
Ideal regimen consists of azithromycin or clarthromycin, rifampin, and ethambutol.
Severe cases may require the addition of streptomycin or amikacin.
In patients with HIV/AIDS antiviral treatment to improve immune status is essential.
Clarithromycin is often considered the macrolide of choice for use in combination therapy for this process, but azithromycin is equally efficacious.
Treatment is generally required for the remainder of the patient’s life.
It may be reasonable to discontinue MAC therapy if patients complete at least 12 months of MAC treatment, have no further symptoms, and demonstrate immune restoration.
Common in patients with advanced AIDS.
Secretion management is focused on chest physiotherapy and expectorants.
Local surgical resection of the lung is an option for treatment resistant disease, depending on the anatomic location and organism pathogenicity.
Typically occurs in elderly women into it to be brought on by voluntary cough suppression which creates a layering of secretions in the lungs providing a medium for infection.
Patients often have a history of bronchiectasis and asthma.
Patients endure symptoms for a long period of time.
Disseminated infections seen in advanced AIDS.
Acquired via the gastrointestinal tract and in immunosuppressed patients adheres to mucosal surfaces and subsequently invades the gut wall.
Organisms multiply in macrophages and are released with cell rupture to local lymphatics and to lymph nodes where further multiplication results in hematogenous dissemination.
Disseminated disease associated with fever and night sweats.
Can involve the gastrointestinal tract and be associated with nausea, diarrhea and weight loss.
Can be associated with abdominal pain, mesenteric lymph node enlargement, retroperitoneal adenopathy, ascites, and peritonitis.
Has a predilection for lymph node involvement of the mesentery and retroperitoneum.
Typically treated with two or three antimicrobial agents for at least 12 months.
Symptomatic patients with pulmonary disease and signs of progression require macrolide-based therapy.
Treatment regimen includes a macrolide, either azithromycin or clarithromycin, rifampin, and ethambutol,for a total of 12 months duration after the first negative sputum results.
Three times per week drug administration is as effective as daily treatment and is associated with better tolerance.
Treatment of adults who have pulmonary disease caused by the most common NTM pathogens.
Included among the slowly growing NTM are Mycobacterium avium complex (MAC), Mycobacterium kansasii, and Mycobacterium xenopi. , and the rapidly growing NTM is Mycobacterium abscessus.
Adding amikacin liposome inhalation suspension to the treatment regimen for patients with MAC pulmonary disease who have failed therapy after at least 6 months of guideline-based therapy.
Consider a macrolide-containing multidrug treatment regimen for patients with M abscessus pulmonary disease caused by strains without inducible or mutational resistance.
Instead of watchfully waiting, initiate treatment for patients who meet the diagnostic criteria for NTM pulmonary disease, especially in the context of positive acid-fast bacilli sputum smears and/or cavitary lung disease.
Consider a regimen of rifampicin, ethambutol, and either isoniazid or macrolide for patients with rifampicin-susceptible M kansasii pulmonary disease.
Consider using a multidrug treatment regimen that includes moxifloxacin or macrolide among patients with M xenopi pulmonary disease.
