Rare diaphragmatic hernia.
Incidence of 1-3% per 10,000 of live births.
Accounts for 2 to 4% of congenital diaphragmatic hernia, and is caused by congenital anterior medial subcostal defects.
Accounts for 3% of congenital diaphragmatic hernias.
2/3 of congenital diaphragmatic hernias can be detected on routine fetal ultrasound, the mean gestational age of diagnosis is 22 to 24 weeks.
Morgagni hernia accounts for approximately 2% of all CDH cases, it is characterized by herniation through the foramina of Morgagni which are located immediately adjacent and posterior to the xiphoid process of the sternum.
Morgagni hernia are rarely identified on fetal ultrasound.
In between 34 and 50% of such hernias are associated with other congenital anomalies such as Down syndrome or AV septal defect.
Approximately 2/3 of patients with Moragagni hernia are symptomatic in infants or childhood and present with respiratory symptoms, such as recurrent chest infections or chronic cough, G.I. symptoms, such as gastric pain, and or nausea and vomiting, or a combination of pulmonary and gastrointestinal symptoms.
Due to its typical small size and sub costosternal defect and location this hernia is rarely identified on fetal ultrasound.
A defect in the diaphragm in the retroxiphoid sternocostal hiatus through which omentum, colon, stomach or other viscera can herniate.
Results from the congenital failure of the diaphragm’s septum tranversum to fuse with costal arches.
Mortality estimates range from 10 to 90% based on severity of the diaphragmatic defect, presence of other congenital, malformations, and access to specialized care.
Most often present later in life as the diaphragm attenuates.
Defect usually located on the right side at the level of the seventh rib on either side of the xiphoid where epigastric vessels pass.
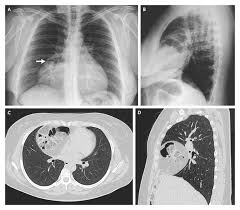
On chest, x-ray a Morgagni hernia typically presents as a radio lucent retrosternal paracardiac opacity, and the bowel is herniated into the chest.
The diagnosis can be confirmed on abdominal CT scan with intravenous contrast.
Left-sided hernia referred to associated a Larrey hernia.
Differential diagnosis includes, pleuropericardial cyst, mesothelioma of the pleura, pericardial fat pad, thymoma, tumor or cyst of the diaphragm.
Diagnosis of such a hernia requires surgical repair.
Surgery can be performed conventionally associated an open approach through the thorax or via laparoscopic approach.
May be associated with congenital abnormalities including Down’s syndrome, Noonan syndrome, Prader-Willi syndrome, Turner syndrome, atrial septic defect and pentalogy of Cantrell.
Approximately 2/3 of patients with Morgagnii hernia are symptomatic in infancy or childhood and present with respiratory symptoms, such as recurrent chest infections or chronic cough, G.I. symptoms, such as gastric pain, and or nausea and vomiting, or combination of pulmonary and gastrointestinal symptoms.
As patients age the diaphragm attenuates and increased abdominal pressure from pregnancy, obesity and trauma leads to presentation.
Patients may be asymptomatic on presentation or have cardiopulmonary symptoms from pressure on intrathoracic organs or pulmonary infections.
Gastrointestinal symptoms may be present as a result of visceral herniation.
Is a direct type hernia and is composed of a sac with omentum, colon, stomach, liver or other gastrointestinal contents.
It may be identified adulthood, presenting with respiratory or G.I. symptoms related to the hernia, or discovered incidentally on imaging studies.
Patients with Morgagni hernia rarely present with intestinal obstruction or respiratory distress requiring emergency surgery.
Following identification, hernia is repaired surgically promptly due to the risk of bowel strangulation and leading to bowel ischemia or perforation.
Minimally, invasive surgical procedures, including laparoscopic and thoracoscopic surgery are preferred approaches for hernia repair.
Placement of the patch of mesh may be considered if the defect is large or under significant tension.
