Mixed connective tissue disease (MCTD) is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP) together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis.
Anti-RNP antibodies develop against RNP when RNP is found outside of the nucleus.
RNP is immunologically protected due to its location, however if a cell dies and RNP is no longer contained in the nucleus and thus unprotected, the immune system can respond by forming antibodies due to cellular mimicry.
Risk to develop MCTD can increase if the body has exposed to molecules or viruses with a similar structure to RNP in the past.
This specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma.
Undifferentiated connective tissue disease, is not necessarily associated with serum antibodies directed against the U1-RNP, and MCTD is associated with a more clearly defined set of signs/symptoms.
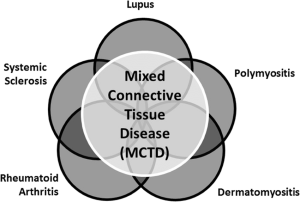
MCTD combines features of scleroderma, polymyositis, systemic lupus erythematosus, and rheumatoid arthritis, myositis, dermatomyositis, and inclusion body myositis, and is thus considered an overlap syndrome.
Its initial clinical manifestations are unspecific: general malaise, arthralgias, myalgias, and fever.
The specific signs of this disease is the presence of positive antinuclear antibodies (ANA), specifically anti-RNP, associated with Raynaud’s phenomenon.
Almost every organ can be affected by MCTD.
Raynaud’s phenomenon is the most common presenting symptom.
Arthralgias and swollen hands are the second and third most common symptoms, respectively.
MCTD most common symptom with arthritis, Raynaud’s, swollen hands, leukopenia/lymphopenia, and heartburn in descending order.
3.6 years is the average amount of time from the first manifestations of the disease until all the criteria for diagnosis are met.
Raynaud’s phenomenon is universal and almost always is present at the beginning of the disease course.
Capillary alterations are similar to that of scleroderma.
Swollen fingers and occasionally diffuse edema are distinctive signs.
Arthritis usually is more frequent and severe than that observed in SLE.
Approximately 60% present have obvious arthritis, with deformities similar to those observed in rheumatoid arthritis.
Myalgias are common.
Pericarditis is the most common cardiac manifestation, observed in 10–30% of patients.
Myocardial involvement, usually secondary to pulmonary hypertension, as well as conduction anomalies may be present.
Pulmonary involvement: Is observed in 75% of patients: pleural effusion, pulmonary hypertension, interstitial lung disease, and thromboembolic disease.
MCTD has an absence of severe renal disease.
The most common gastrointestinal change is the alteration of esophageal motility like that observed in scleroderma.
There is an absence of changes to the CNS; but trigeminal neuropathies of the cranial nerve V, and sensorineural hearing loss, and headaches have been observed in patients with MCTD.
Mild anemia and hypergammaglobulinemia are common, other hematologic anomalies such as those observed in SLE can also be observed.
Rheumatoid factor is positive in 50–70% of patients, and anti–citrullinated protein antibody is detected in 50% of patients.
Universal serological findings in patients with MCTD is the presence of anti-nuclear antibody, with anti-nRNP specificity, especially antibodies against protein 68 kD.
There are currently no known environmental factors or triggers contributing to MCTD.
It has been associated with HLA-DR4.
DIAGNOSIS:
Key laboratory characteristics are a positive, speckled anti-nuclear antibody and an anti-U1-RNP antibody.
Some clinical manifestations make it more likely to suspect the disease is MCTD over other connective tissue diseases:
Raynaud’s phenomenon.
Edematous hands and swollen fingers.
Arthritis more severe than that of SLE.
Pulmonary hypertension
Anti-RNP antibodies in elevated levels, especially antibodies against protein 68 kD.
Absence of severe renal or CNS disease.
There is no agreement exists as to what the optimal criteria are for diagnosis.
Even with a low anti-RNP antibody titer, a patient can show symptoms of MTD, and
a patient with a high anti-RNP antibody titer can have no symptoms.
Criteria require the presence of high titres of anti-RNP antibodies, the presence of some characteristic signs of the disease – Raynaud or swollen hands/fingers – and the presence of some clinical manifestations of at least two other connective tissue diseases – SLE, scleroderma, polymyositis.
A. Serologic criteria:
Positive Anti-RNP at a titre> 1:1600 by hemagglutination
B. Clinical Criteria
1. Edema of the hands
2. Synovitis
3. Myositis
4. Raynaud’s phenomenon
5. Acrosclerosis
MCTD is present with:
Criteria A together with 3 or more clinical criteria! one of which must be synovitis or myositis.
The presence of the specific antibody anti-U1 RNP is the sine qua non for the diagnosis of MCTD.
If the dominant autoantibodies are antiDNA, Sm, Scl70 or Ro, it is likely the patient will develop another connective disease distinct from MCTD.
The clinical manifestations of MCTD appear correlated more intensely to the antibodies against protein A’ and 68 kD of the U1 RNP complex.
MCTD is associated with HLA-DR4 or HLA-DR2.
SLE is associated with HLA-DR3 and those with scleroderma are associated with HLA-DR5.
Antibodies against anti-U1-snRNP are present in most MCTD patients but are seen in only 30–35% of SLE and 2–14% of scleroderma patients.
There are different haplotypes of SNRNP70 which due to their differences in patients with MCTD versus those with SLE or scleroderma.
The T-G-CT-G haplotype is more common in patients with MCTD, whereas the T-G-C-G haplotype is more commonly seen in scleroderma and SLE.
TREATMENT: based on the specific manifestations and clinical complications,.
For arthritis, non-steroidal anti-inflammatories or low dose prednisone are usually used, which can be used in association with methotrexate or hydroxychloroquine.
Higher doses of corticosteroids (0.25 to 1 mg/kg/day) are used in complications such as myositis, meningitis, pleuritis, pericarditis, myocarditis, interstitial lung disease, or hematologic abnormalities.
Raynaud’s phenomenon, acrosclerosis or peripheral neuropathies are usually resistant to corticosteroids.
Cyclophosphamide is used in interstitial lung disease and in the event of serious renal involvement.
Myositis, and refractory thrombocytopenia resistant to corticosteroids, May be treated with intravenous immunoglobulins.
For Raynaud’s tobacco cessation, protection against the cold, calcium antagonists, endovenous prostaglandins or endothelin-2 antagonists may be used.
In patients with gastroesophageal reflux, proton pump inhibitors can be used.
Early diagnosis of pulmonary hypertension, the major cause of death, by routine echocardiography and the rapid initiation of treatment with endothelin-1 antagonists, phosphodiesterase 5 inhibitors or endovenous prostacyclins improve morbidity and mortality.
Survival rates at 5, 10, and 15 years are 98%, 96%, and 88% respectively, with the main causes of death being pulmonary hypertension, cardiovascular problems, and infections.
The presence of anticardiolipin antibodies as well as the presence of more scleroderma and polymyositis signs and symptoms is associated with more serious disease.
Morbidity is quite high in patients with MCTD.
The prognosis of mixed connective tissue disease in one third of cases is worse than that of systemic lupus erythematosus (SLE).
In these individuals disease is progressive and may in many cases evolve into a progressive systemic sclerosis (PSS), which has a poor outcome.
30% of cases the disease is mild and may require only aspirin as treatment, and may go into remission where there is no anti-U1-RNP antibodies detected.
Most deaths from MCTD are due to heart failure caused by pulmonary arterial hypertension.
MCTD may progress to a clinical picture more consistent with other connective tissue diseases like SLE, scleroderma, or rheumatoid arthritis.
MCTD May require reclassification over time with other diseases: rheumatoid arthritis in 9%, SLE in 15%, and scleroderma in 21% of cases.
Such progression of disease is determined genetically, thus SLE is more likely in patients with HLA-DR3 and scleroderma in patients with HLA-DR5.
The prevalence of MCTD is higher than that of dermatomyositis and lower than that of SLE.
A Norwegian study, the prevalence of MCTD was 3.8 per 100,000 adults, with an incidence of 2.1 per million per year.
MCTD is much more frequent in women than in men at between a 3:1 to 16:1 ratio, and in women younger than 50.
The general age at onset is around 15–25 years old.
