 Subset of diffuse large B cell lymphoma with predominant mediastinal involvement, with clear cytoplasmic cells, with convoluted or centroblastic nuclei and thin bands of sclerosis.
Subset of diffuse large B cell lymphoma with predominant mediastinal involvement, with clear cytoplasmic cells, with convoluted or centroblastic nuclei and thin bands of sclerosis.
Primary mediastinal B cell lymphoma is a rare, but aggressive, mature B cell lymphoma arising from thymic B cells.
Represents 2 to 4% of non-Hodgkin’s lymphoma with a predominant among females.
Expresses B cell surface antigens CD20 and CD79a and IgH rearrangement and mutations.
CD 30 and CD 23 o are expressed in 77% and 67%, respectively, of childhood cases of primary mediastinal B cell lymphoma.
Expression of CD30 is more common in primary mediastinal large B-cell lymphoma than in other types of large B-cell lymphoma.
Like Hodgkin’s disease, it has a peak incidence in adolescents and young adults, presenting as a mediastinal mass, alterations in nuclear factor-kB and JAK/STAT signaling, and up regulation of PD-L1..
It is an aggressive C-cell lymphoma and its molecular signature is more like Hodgkin’s lymphoma rather than DLBCL (diffuse large B-cell lymphoma), and is characterized by activation of NFkB and JAK-STAT pathways and program death ligand 1 and 2 overexpression.
At the molecular level, alterations in Janus/signal transducers and activators of JAK-STAT transcription pathways.
Often has copy number alterations and rearrangements of 9p24.1.
Cells usually do not have surface IgG.
PD-1 expression in 70% of patients.
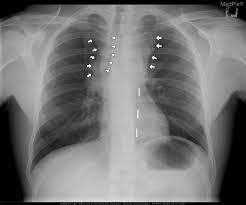
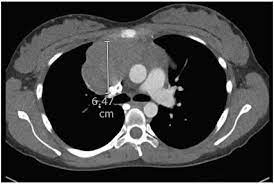
Typically presents with bulky mediastinal disease and can be associated with pleural and pericardial effusions.
It is a highly aggressive tumor, with a rapid growing mediastinal mass, usually bulky, which frequently causes a superior vena cava syndrome, other compressive symptoms, and pleural and pericardial effusions.
Most patients are diagnosed with early disease.
Rarely it is more extensive at the time of diagnosis involving extranodal sites such as the kidneys, adrenals, stomach, and ovary.
It usually does not involve the bone marrow or CNS initially.ee
Involvement of extranodal sites or the CNS is more frequent at the time of relapse/progressive disease.
Patients are often young and female.
Patients typically present with symptoms related to mediastinal bulky masses, which involve the chest wall, lung, pleura or pericardium.
Many patients have associated plural of pericardial effusions.
Bone marrow or CNS involvement are uncommon initially, and elevated levels of LDH and overt B symptoms can occur.
Diagnosis is a preferred excisional biopsy, but this is often not feasible, because of the respiratory and cardiac compromise.
A needle image guided percutaneous biopsy is appropriate.
Disease staging includes bone marrow aspiration, bone marrow biopsy, lumbar puncture, PET/CT scans and rapid initiation of therapy.
Approximately 20% ofpatients present with stage 3 or 4 disease.
Metastatic disease can involve the kidneys and adrenal glands.
Prognosis is good, with approximately 90% of patients cured with modern therapy.
Prognosis indicated by the International Prognostic Index (IPI), with high IPI patients having a worse prognosis than low IPI patients.
Biopsy is required for diagnosis, to rule our other types of lymphoma.
Clinically may be associated with a superior vena cava syndrome and pleural effusions.
In symptomatic patients treatment needs to start quickly.
Traditionally treated with CHOP or combination chemotherapy with eoposide, leucovorin, doxorubicin, cyclophosphamide, vincristine, prednisone and bleomycin, followed by radiotherapy.
To avoid radiotherapy newer approaches with rituximab, etoposide, doxorubicin, cyclophosphamide, vincristine and prednisone alone have been highly successful.
Treatment with rituximab, cyclophosphamide, doxorubicin vincristine and prednisone followed by radiation produces cure rate between 75 and 80% and long-term survival of 85-90%.
For patients with primary mediastinal B-cell lymphoma (PMBCL) who achieved a complete metabolic response after immunochemotherapy, radiation therapy may be safely omitted without heightening their risks of relapse or disease progression – thereby sparing them the toxicity and costs of this additional treatment.
Recurrent or refractory patients have a poor prognosis.
Checkpoint inhibitors associted with good responses for refractory patients.
Primary B cell mediastinal lymphoma is radiosensitive, however, its role is not clear given the effectiveness of intensive chemotherapy.
The role of PET/CT scans in evaluating end of treatment plans has not yet been clarified.
Circulating tumor, DNA (ctDNA) is a potential biomarker for the diagnosis, prognosis, response, assessment, and remission monitoring.
Most patients who do not experience a response to initial treatment will experience will disease progression.
Recurrent disease commonly occurs within eight months of the initiation of therapy and with more than half of progressions occurring in less than one year.
Sites of relapse, including the mediastinum with new or extranodal disease, the lung liver, kidney, and adrenal glands.
CNS disease is rare at initial presentation, but may occur later in the disease.
Refractory and relapse patients require additional aggressive combination chemotherapy followed by consolidation with high-dose chemotherapy and autologous stem cell transplant that can result in an overall survival rate of 65 to 68%.
Checkpoint inhibitors, BTK inhibitors, and anti-CD 19 CAR T cell therapy are being investigated for relapse and refractory disease.
