A lymph node is an organized collection of lymphoid tissue, through which the lymph passes on its way back to the blood.
A lymph node is an organized collection of lymphoid tissue, through which the lymph passes on its way back to the blood.
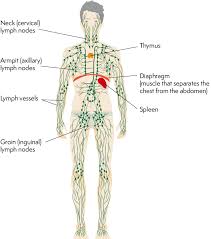
Lymph nodes are located at intervals along the lymphatic system.
Lymph nodes are a part of the reticuloendothelial system, which includes monocytes of the blood, macrophages of the connective tissue, thymus, spleen, bone marrow, bone, mucosa-associated lymphoid tissue of visceral organs, lymphatic vessels, and lymphatic fluid found in interstitial fluid.
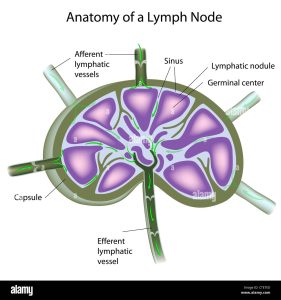
Surrounded by a capsule composed of connective tissue and elastic fibrils.
Foreign substances are presented to the lymphoid cells, which may lead to cellular proliferation and enlargement: cellular proliferation in lymphoid follicles may be identified as several mitotic figures.
As lymphatic capsules stretch due to increased activity, patients may experience localized tenderness.
The capsule is perforated by afferent lymphatics that empty into a fenestrated subcapsular peripheral sinus.
Several afferent lymph vessels bring in lymph, which travels through the substance of the lymph node, and is then drained out by an efferent lymph vessel.
Lymph extravagates from the peripheral sinus to the lymph node collecting in medullary sinusoids and exiting through a single efferent lymphatic vessel in the hilus, which is also the site of the penetration of the single small artery and vein.
Primary follicles are aggregates of small lymphocytes in the cortex subjacent to the peripheral sinus and they contain numerous immunologically naive B cells.
The paracortical area lies between the primary follicles and contains numerous T cell lymphocytes.
The medulla, lies deep to the cortex and contains plasma cells and few lymphocytes.
Of the nearly 800 lymph nodes in the human body, about 300 are located in the head and neck.
Groups of lymph nodes are in clusters in different regions, as in the underarm and abdominal areas.
Lymph node clusters are commonly found at the proximal ends of limbs (groin, armpits) and in the neck, where lymph is collected from regions of the body likely to sustain pathogen contamination.
Lymph nodes are numerous in the mediastinum in the chest, neck, pelvis, axilla, inguinal region, and in association with the blood vessels of the intestines.
Constantly respond to stimuli, including infectious agents, even if clinical symptoms are absent.
Lymphatic fluid moves throughout the lymphatic system, transitioning from the organs to lymphoid capillaries, lymphatic vessels, and finally lymph nodes for foreign antigen filtration.
Following antigenic stimulation the primary follicles enlarge and transform into germinal centers.
The substance of a lymph node consists of lymphoid follicles in an outer portion called the cortex.
The inner portion of the node is called the medulla, which is surrounded by the cortex on all sides except for a portion known as the hilum.
The hilum presents as a depression on the surface of the lymph node.
The hilumcauses the otherwise spherical lymph node to be bean-shaped or ovoid.
Germinal centers are dynamic structures where B cells respond to antigens by making antibodies.
Normal germinal centers are surrounded by a darker staining area the mantle zone, which contains small naive B cells.
In nodes reactive to some types of conditions a rim of B cells accumulate outside the mantle zone and are referred to as marginal zone B cells.
Paracortical T cell zones can undergo hyperplasia as a result of stimulation of cellular immunity.
Localized lymphadenopathy is common and 55% of cases involve lymph nodes in the head and neck region.
Of all cases of lymphadenopathy 1% or related to supraclavicular lymph nodes, 5% to axillary lymph nodes and 14% to inguinal lymph nodes.
There is approximately 600 lymph nodes in the human body.
Lymph nodes are divided into groups that serve individual anatomical sites.
Lymphadenopathy is evaluated as to size, rate of growth, tenderness, and consistency.
Lymph node size is the most important characteristic of lymphadenopathy, and lymph nodes less than 1 cm in diameter does not usually reflect the presence of malignancy.
In assessing lymphadenopathy, age is the most helpful variable: Patients who are 40 years of age or older have a 4% risk of cancer, whereas younger patients less than 40 years of age have a 0.4% risk.
Common causes of lymphadenopathy include infections: dental abscesses, otitis media, otitis externa, pharyngitis, scalp infections, toxoplasmosis, Epstein-Barr virus, cytomegalic virus, adenovirus, hepatitis, rubella, tuberculosis, Bartonella infection.
Cancer causes of lymphadenopathy include: non-Hodgkin’s lymphoma, Hodgkin’s disease, head and neck cancer, and unicentric Castleman’s disease.
Autoimmune disease relation to lymphadenopathy includes systemic lupus erythematosus.
Other diseases associated with lymphadenopathy include sarcoidosis.
Tumor involvement portends and adverse effect on survival for many cancers including breast colon, esophagus, stomach and pancreas.
Routine histopathology samples about 1% of a submitted nodal tissue specimen.
Lymph node counts have been proposed as a metric to assess adequacy of surgical resection and or pathologic examination and thresholds of a minimum lymph node count have been required for inclusion in the number of clinical trials.
Detection of very small metastatic deposits (1 to 3 cells) by routine histopathologic examination of lymph nodes statistically will be possible only in 1% of evaluated patients.
Number of pathologically negative nodes correlates with survival in melanoma, breast and rectal cancers.
Number of pathologically negative nodes correlates with survival in melanoma, breast and rectal cancers.
More extensive lymph node sampling may contribute to survival in endometrial cancer.
Only 23.2% of patients with gastric cancer and 16.4% of patients with pancreatic cancer in the U.S. underwent evaluation of at least 15 lymph nodes.
Nodal examination is important for staging and adjuvant therapy decision making and high volume hospitals have improved long-term outcomes for gastric and pancreatic cancers as a result of more vigorous lymph node evaluations.
