 Microscopic examination for cellular morphology and architecture, special stains and cultures are performed on the tissue obtained to achieve diagnosis.
Microscopic examination for cellular morphology and architecture, special stains and cultures are performed on the tissue obtained to achieve diagnosis.
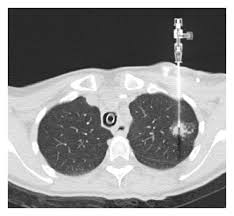
A lung biopsy can be performed percutaneously, typically guided by a CT Scan, via bronchoscopy with ultrasound guidance, or by surgery, either open or by video-assisted thoracoscopic surgery (VATS).
A lung biopsy is performed when a lung lesion requires identification.
A lung biopsy risk includes a pneumothorax.
This risk, which ranges from 1% to about 10%.
The precise risk of pneumothorax depends on the biopsy technique and on underlying lung disease.
Certain lung diseases such as COPD can increase the risk of pneumothorax.
Pneumothorax may require treatment with a chest tube.
Bleeding can occur in 1 to 4%, of patients and can be life threatening.
Lung biopsy is a widely accepted procedure for diagnosing pulmonary disorders: lung nodules and masses, interstitial lung diseases, hypersensitivity pneumonitis, sarcoidosis, and infections.
Lung tissue can be obtained for histopathological examination via the following methods:
Percutaneous Transthoracic Lung Biopsy (PTLB).
In PTLB, also be referred to as a percutaneous or transthoracic needle biopsy in which a needle is inserted through the chest wall via CT or fluoroscopic guidance into the suspected area to obtain a tissue sample.
Open Lung Biopsy (OLB).
Surgical removal of lung tissue for histopathological and microbiological analysis under general anesthesia.
Video-Assisted Thoracic Surgery (VATS) refers to endoscopic removal of lung tissue via the chest wall.
Transbronchial Biopsy uses a flexible bronchoscopy via the transnasal or transoral route usually preferred for central accessible lesions.
Bronchopulmonary segments are independent units of the lung supplied by a tertiarysegmental bronchus, a tertiary branch of the pulmonary artery, and a branch of the bronchial artery.
There are ten bronchopulmonary segments in the right and 8 in the left lung, respectively.
The right lung has oblique and horizontal fissures dividing it into three lobes with ten segments.
Right Upper Lobe
Apical segment
Posterior segment
Anterior segment
Right Middle Lobe
Lateral segment
Medial segment
Right Lower Lobe
Lymph node locations are mapped into 14 stations and seven zones according to their relation to various surgical landmarks like the trachea, bronchi, pleura, great vessels.
Supraclavicular Zone
Station 1
Upper Zone (Superior Mediastinal Nodes)
Station 2 (upper paratracheal)
Station 3 (prevascular, retrotracheal)
Station 4 (lower paratracheal)
Aortic Nodes
Station 5 (subaortic)
Station 6 (para-aortic)
Inferior Mediastinal
Station 7 (subcarinal)
Station 8 (para-esophageal)
Station 9 (pulmonary ligament)
N1 nodes
station 10 (hilar)
station 11 (interlobar)
station 12 (lobar)
station 13 (segmental)
station 14 (subsegmental)
The thoracic wall consists of the rib cage that forms the bony skeleton wall and the skin, the underlying muscles, and fascia.
From superficial to deep, the chest wall contains the following layers:
Skin
Superficial fascia
Deep fascia
Serratus anterior
Ribs and intercostal muscles
Endothoracic fascia
A lung biopsy is required when there is a need to provide a specific diagnosis.
Indications for PTLB.
New or enlarging mass or solitary nodule on chest radiography that is not
diagnosable by CT or is unlikely to be accessible by bronchoscopy.
Multiple nodules in a patient with no previous history of malignancy.
Persistent focal infiltrates for which no diagnosis has been made by sputum, or bronchoscopy, blood culture, serology.
Hilar mass.
Transtracheal needle biopsy (TTNB) is indicated for evaluating an undiagnosed pulmonary nodule or mass, and is also useful for the evaluation of mediastinal masses, hilar masses that are undiagnosed post bronchoscopy, and also for the diagnoses of infective diseases presenting as nodules or consolidation.
Transbronchial biopsy (TBLB) is useful for diffuse and localized pulmonary disorders and is often the primary diagnostic modality for centrilobular lesions like sarcoidosis, interstitial lung disease, hypersensitivity pneumonitis, eosinophilic pneumonia or infective etiology like tuberculosis, or lung disease of unclear etiology is suspected.
VATS has lesser complications and early recovery. It is indicated for mediastinal lymph node biopsy, pleural biopsy, a biopsy of lung tissue/lymph node, and undetermined interstitial lung disease.
Open or surgical biopsy (OLB) has been considered as the gold standard for the diagnosis of lung parenchymal lesions. However, a trial of a less invasive method is usually preferred unless any major contraindications and OLB.
Relative contraindications for PTLB:
The previous history of pneumonectomy
Severe emphysematous disease,
Presence of bullae that obstruct the path of biopsy
Patients with intractable cough,
Patients on mechanical ventilation
Pulmonary hypertension.
Bleeding diathesis that is uncorrectable before the procedure
Severe hypoxemia, uremia, and thrombocytopenia.
Recent MI,
VATS is contraindicated for patients with the inability to tolerate single lung ventilation.
Several options for percutaneous lung biopsy needles are available, including aspiration and cutting needles.
The choice of the needle also depends upon the size of the lesion, needle trajectory, and operator preference.
The procedure is performed with detailed imaging under fluoroscopic or CT guidance.
A cytopathologist should be available for the procedure and check for the adequacy of the sample.
Transbronchial Biopsy:
Essential equipment includes a flexible bronchoscope with a light source and video monitoring.
Tissue samples are taken with the help of biopsy forceps.
Suction apparatus, oxygen supply and also, equipment to provide cardiopulmonary resuscitation must be available.
VATS procedure includes a video thoracoscope, diathermy pen, sponge holding, and biopsy forceps, endoscopic staple transaction devices, rigid or flexible trocar cannula, thoracotomy tray, chest tube with water seal, and suction source with tubing.
VATS: Anesthesia is administered in a supine position before the procedure, and a double-lumen tube (DLT) is the airway of choice.
Three incisions are made in the anterior approach, and classically three ports are created, including the camera and operating ports, which are checked with the video thoracoscope.
Pain control, respiratory and chest tube care must be provided post-operatively.
An Open Lung Biopsy is an invasive operative procedure, that is done under general anesthesia.
Coagulation indices, including prothrombin time (PT), activated partial thromboplastin time (APTT), platelet counts should be evaluated before the procedure.
Oral anticoagulants must be stopped before the procedure.
Under general anesthesia with the patient in the supine position, an incision is made 2-3cm lateral to the nipple line.
The pleura is entered between the fifth and sixth rib, and blunt dissection is carried out to bring the lung tissue in the operating field.
Complications:
Pneumothorax is the most common complication.
Hemoptysis, pulmonary hemorrhage, pulmonary venous air embolism, and a large hemothorax cause mortality from percutaneous transbronchial lung biopsy (PTLB).
Pneumothorax is the most common complication.
Pneumothorax, pulmonary hemorrhage, hemothorax, cardiac tamponade, and seeding along with the needle tract cause morbidity.
In a transbronchial biopsy, reaction to the topical anesthetic, ET tube induced trauma, laryngospasm, bronchospasm, hypoventilation, pneumothorax, and hemorrhage can occur.
Open lung biopsy is performed under general anesthesia with the patient in the supine position, an incision is made 2-3cm lateral to the nipple line.
Biopsy samples are sent to the histopathologist.
Open lung biopsy complications include:
massive hemoptysis, pulmonary hemorrhage, pulmonary venous air embolism, hemothorax, cardiac tamponade, and tumor seeding.
When compared with fine needle aspiration, core biopsy has been shown to have a slightly higher overall sensitivity, specificity, and accuracy with an improvement in the definitive diagnosis of benign lesions.
Core biopsy is not recommended for lesions <10 mm due to the increased complication rates and decreased diagnostic accuracy.
Transbronchial lung biopsyis an accepted method for lung biopsy for a wide array of diseases, including ILD’s, vascular diseases, small airway diseases, and malignancies.
Has a low overall mortality of 0.1% compared to surgical lung biopsy (1%).
Does not require general anesthesia and can be done as an outpatient procedure.
While it can be used for centrally accessible lesions, it is not as sensitive as a percutaneous biopsy for lesions less than 2cm.
Percutaneous, and surgical lung biopsy has a superior diagnostic yield.
Cryo-TBB is safe and generally free of major complications. Besides the risk of massive bleeding, post-procedure pneumothorax ranges from 2.6 to 30 %, moderate bleeding from 4 to 78 %, and rarely death (0.3 %) have been reported.
Although VATS has been preferred over surgical lung biopsy, there are situations like severe pleural disease, anticipated bleeding, or more severe respiratory impairment that favor the use of SLB-thoracotomy.
Patients with severe hypoxemia or mechanical ventilation are not good candidates for VATS, as it requires a period of single lung ventilation.
Recent advances in interventional pulmonology have further revolutionized the diagnosis of lung masses, nodules, lymphadenopathy, and pleural diseases. Newer diagnostic modalities like convex probe (CP) and radial probe (RP) EBUS (endobronchial ultrasound), ENB (electromagnetic navigational bronchoscopy), Cone beam CT and robotic bronchscopy are now available.
The yield of these newer modalities is comparable to that of CT guided biopsy with lesser complications.
These interventions help in the early diagnosis and management of the patients.
Image
Table
Enhancing Healthcare Team Outcomes
As discussed earlier, the decision to undergo lung biopsy and the specific type of procedure must be made by a multidisciplinary team, comprising of a radiologist, surgeon, and chest specialist.[3]
Nursing, Allied Health, and Interprofessional Team Monitoring
Post-procedure monitoring of vitals is essential by the nursing staff for several hours after the procedure and appropriate chest tube care if present.
Broncoscopic methods are associated with lower rates of pneumothorax: rates of 2 to 6% for transbronchial lung biopsy and less than 1% for endobronchial ultrasound guided transbronchial needle aspiration compared with percutaneous fine needle aspiration which is associated with a risk of pneumothorax in approximately 17 to 26% of biopsies.
Bronchoscopy is less invasive and less expensive than surgical mediastinoscopy.
Surgical lung biopsy is rarely warranty warranted given the high yield, lower cost and lower rates of adverse outcomes for bronchoscopic techniques.
