 Multiple clinical trials confirm equivalence of overall survival outcomes between breast conserving surgery and mastectomy for operable breast cancer.
Multiple clinical trials confirm equivalence of overall survival outcomes between breast conserving surgery and mastectomy for operable breast cancer.
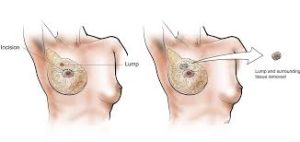
The major complication is failure to excise the mammographic or palpable target and occurs in fewer than 3% of cases.
Almost three times as much normal tissue is excised when a needle localization is used to identify a mammographic target with calcifications as when there is a palpable mass that is removed.
30-40% of surgically grossly resected breast cancer masses with negative surgical margins will still have microscopic residual disease that can develop into the recurrent disease (Fisher B).
About one fourth of women who undergo lumpectomy need to have one or more additional surgeries to remove malignant tissue to ensure tumor negative margins.
No ink on tumor is the definition of clear margins in patients treated with lumpectomy and RT.
Standard acceptable lumpectomy margins is clearance of tumor inked surfaces.
A preoperative diagnosis of cancer by a core needle biopsy compared to a needle localization and excision biopsy is associated with the removal of more breast tissue with the lumpectomy in the former than in the later technique.
Imaging is essential for determining patient eligibility for lumpectomy.
Preoperative bilateral mammograms are done to evaluate the size of the primary lesion, evidence of multi centric disease, the extent of malignant micrrocalcifications, and possible contralateral synchronous breast cancer.
Findings of difuse malignant calcifications and or calcifications tha cannot be encompassed by a lumpectomy specimen should undergo mastectomy.
Lumpectomy in a patient with cancer associated microcalcifications it is necessary to obtain a post lumpectomy mammogram to confirm adequacy of resection.
The finding of residual microcalcification is an indication for additional breast surgery which includes re–excision lumpectomy or mastectomy regardless of whether margin control was achieved with the prior lumpectomy.
Lumpectomy in conjunction with the axillary surgery as initial treatment provides to patient and multidisciplinary team definitive histopathology regarding the primary tumor and lymph nodes.
Patients who undergo lumpectomy and are shown to have metastatic disease in one or two lymph sentinel lymph nodes can usually be spared from undergoing a completion axillary lymph node dissection.
Commonly excepted guidelines suggest it can be safely offered to patients with T1 and T2 breast cancers.
Widely accepted that patient eligibility for lumpectomy is determined more by anticipated cosmetic result, the ability to achieve margin control and deliver adjuvant radiation, than by arbitrarily selected threshold of the size of the primary tumor.
Tumor location and other features related to anatomy for an individual patient may influence the acceptability of lumpectomy.
Body habitus and tumor volume ratio have an impact on choice of surgical therapy:in the patient with relatively small breasts, conservative therapy may yield an unsatisfactory cosmetic result given the breast volume loss secondary to a margin negative lumpectomy and tissue retraction due to radiation related fibrosis.
On the other hand, T3 cancer may be amenable to breast conserving therapy in a large and pendulous breasts.
Morbid obesity may preclude eligibility for lumpectomy because radiation therapy facilities have a weight limit.
ACS Oncology Group Z0011 trial demonstrated that completion axillary lymph node dissection provides no advantage in clinical outcomes to patients with one or two positive sentinel nodes are present, and observed equivalence of locoregional control likely related to adjuvant radiation of the lower nodal basin of the breast.
The quality of the cosmetic outcome may not become apparent until 2-3 years after the completion of radiation therapy when scar retraction at the surgical site is complete.
Adequate surgical excision depends on accurate preoperative localization and failure to localize, excise or identify the excised lesion occurs in 2-4% of cases.
Associated with the lowest negative impact on sex life at 29.8% compared to 45.4% among women that have undergone modified radical mastectomy with reconstruction.
Adjuvant radiation does not have a significant impact on overall survival, but it reduces the risk of in- breast recurrence substantially.
Lumpectomy followed by whole- breast radiation is associated with an average annual risk of subsequent in-breast cancer events ranging from 0.3% to 1% and at five years local recurrences are observed in 2-5% of cases.
During the first 5-10 years of follow up, most in-breast events are true local recurrences, and increased risks present progressive likelihood of developing a new primary breast cancer over time.
MRI performed in patients with newly diagnosed breast cancer leads to higher rates of mastectomy.
MRI procedures prior to breast conservation surgery fails to demonstrate reduced rates of Local recurrence or reexcision.
