 The loop electrosurgical excision procedure (LEEP) is a commonly used approaches to treat high grade cervical dysplasia (CIN II/III, HGSIL) discovered on colposcopic examination.
The loop electrosurgical excision procedure (LEEP) is a commonly used approaches to treat high grade cervical dysplasia (CIN II/III, HGSIL) discovered on colposcopic examination.
LEEP has many advantages including low cost and a high success rate.
Management option for the treatment of cervical dysplasia.
Efficacy rates are comparable to those of ablative techniques.
Removes less tissue, associated with less bleeding, pain and infections than conventional surgery.
The prodeure can be done in an office setting and usually only requires a local anesthetic, though sometimes IV sedation or a general anesthetic is used.
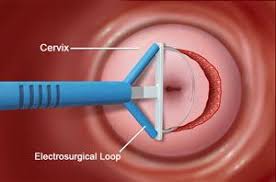
When performing a LEEP, a wire loop is used through which an electric current is passed at variable power settings.
Loops with varying shapes and sizes can be used depending on the size and orientation of the lesion.
The cervical transformation zone and lesion are excised to an adequate depth, which in most cases is at least 8 mm, and extending 4 to 5 mm beyond the lesion. A second pass with a more narrow loop can also be done to obtain an endocervical specimen for further histologic evaluation.
The LEEP technique results in some thermal artifact in all specimens: but this does not generally interfere with pathological interpretation.
Complications are less frequent in comparison to a cold-knife conization but can include infection and hemorrhage.
Associated with premature rupture of membranes in women undergoing subsequent pregnancies.
Associated with preterm delivery.
Positive margins on LEEP specimens reflect an increase risk for recurrence of cervical dysplasia, particularly when high-grade lesions are seen at the margin.
In high income countries women with CIN grade 2 and higher are often treated with loop electrical surgical excision procedure, which excises the transformation zone and histologic abnormalities.
The LEEP procedure does not appear to affect fertility.
Women with a time interval from LEEP to pregnancy of less than 12 months compared with 12 months or more were at significantly increased risk for miscarriage, with risk of miscarriage of 18% compared with 4.6%, respectively.
A large meta-analysis concluded that women with CIN have a higher baseline risk for preterm birth than the general population and that LEEP as the treatment for CIN probably increase this risk further. The risk of preterm birth appears to increase with multiple treatments and increasing amounts of tissue removed.
A study found that women reported a statistically significant decrease in sexual satisfaction following LEEP.
