
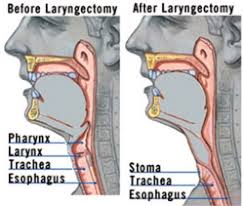
 Laryngectomy refers to the removal of the larynx and separation of the airway from the mouth, nose and esophagus.
Laryngectomy refers to the removal of the larynx and separation of the airway from the mouth, nose and esophagus.
In a total laryngectomy, the entire larynx is removed including: the vocal folds, hyoid bone, epiglottis, thyroid and cricoid cartilage and a few tracheal cartilage rings.
In a partial laryngectomy, only a portion of the larynx is removed.
Following a laryngectomy, breathing occurs through a stoma in the neck.
This procedure is usually performed by an ENT surgeon.
A laryngectomy is performed when treatments for laryngeal cancer fail to conserve the larynx or when the cancer has progressed such that normal functioning would be prevented.
Laryngectomies are also performed on individuals with other types of head and neck cancer.
Post-laryngectomy rehabilitation includes voice restoration, oral feeding and more recently, smell and taste rehabilitation.
International Agency for Research on Cancer, there were 177,422 new cases of laryngeal cancer worldwide in 2018 (1.0% of the global total.)
Among worldwide cancer deaths, 94,771 (1.0%) were due to laryngeal cancer.
In 2019 it is estimated that there were12,410 new laryngeal cancer cases in the United States per 3.0 per 100,000.
The number of new cases decreases every year at a rate of 2.4%, and this is related to decreased cigarette smoking in the general population, and due to the development of less invasive techniques.
To determine the severity/spread of the laryngeal cancer and the level of vocal fold function, indirect laryngoscopies using mirrors, endoscopies (rigid or flexible) with biopsies may be performed.
Imaging using CT scans, MRIs and PET scans and investigations of the cancer through biopsy can also be completed.
Acoustic observations can also be utilized, as certain laryngeal cancer locations can cause hoarseness.
Staging classifications are from T1 to T4 indicating the spread/size of the tumor and provides information on which surgical intervention is recommended.
T1-T3 lesions may require partial laryngectomies and T4 tumors may require complete laryngectomies.
Radiation and/or chemotherapy may also be used.
After a total laryngectomy, breathing occurs through a stoma where the tracheostomy has created an opening in the neck., and there is no longer a connection between the trachea and the mouth and nose.
After a partial laryngectomy, breathing occurs mainly through the stoma, however a connection still exists between the trachea and upper airways such that these individuals are able to breathe air through the mouth and nose (partial neck breathers).
Ventilation and resuscitation of total and partial neck breathers is performed through the stoma.
The most frequent postoperative complication of laryngectomy is pharyngocutaneous fistula (PCF).
A pharyngocutaneous fistula is characterized by an abnormal opening between the pharynx and the trachea or the skin resulting in the leaking of saliva outside of the throat.
A pharyngocutaneous fistula requires nasogastric tube feedings, increases morbidity, length of hospitalization, and level of discomfort, and may delay rehabilitation.
A pharyngocutaneous fistula complicates 29% of persons who undergo total laryngectomy.
Risks for a pharyngocutaneous fistula are related to anemia, hypoalbuminaemia, poor nutrition, hepatic and renal dysfunction, preoperative tracheostomy, smoking, alcohol use, older age, chronic obstructive pulmonary disease and localization and stage of cancer.
Use of a free-flap significantly reduces the risks of pharyngocutaneous fistula.
Complications: wound infection, dehiscence and necrosis, bleeding, pharyngeal and stomal stenosis, and dysphagia have also been reported with laryngectomy.
The removal of the larynx results in loss of sound production.
The loss of voice and efficient verbal communication has a significant impact on the quality of life.
Voice rehabilitation is important for the recovery process following the surgery.
Voice restoration methods are selected based on each individual’s abilities, needs, and lifestyle.
Pre and post-operative sessions with a speech-language pathologist (SLP) are often part of the treatment plan for people undergoing a total laryngectomy.
For tracheoesophageal speech, a voice prosthesis is placed in the tracheo-oesophageal puncture (TEP) created by the surgeon.
The voice prosthesis is a one-way air valve that allows air to pass from the lungs/trachea to the esophagus when the stoma is covered, where the redirected air vibrates the esophageal tissue to produce a hoarse voice.
The tracheo-oesophageal puncture and voice prosthesis combination allows individuals post-laryngectomy to have a voice to speak, while also avoiding aspiration of saliva, food or other liquids.
An electrolarynx is an external device that is placed against the neck and creates vibration that the speaker then articulates.
The sound is mechanical and robotic.
Esophageal speech is a process that the speaker pushes air into the esophagus and then pushes it back up, articulating speech sounds to speak.
It is time-consuming. difficult to learn and is less frequently used.
For individuals using tracheoesophageal or esophageal speech, botulinum toxin may be injected to improve voice quality when spasms or increased tone is present at the level of the pharyngoesophageal segment muscles.
The laryngectomy surgery results in anatomical and physiological changes in the larynx and surrounding structures altering swallowing and compromising the patient’s oral feeding ability and nutrition.
Following a laryngectomy, most patients recover swallowing function within 3 months.
Laryngectomy patients may experience difficulty swallowing solid food, changes in appetite due to a significant loss in their senses of taste and smell.
In order to prevent the development of pharyngocutaneous fistula, it is common practice to reintroduce oral feeding as of the seventh to tenth day post-surgery.
Pharyngocutaneous fistula typically develops before the reintroduction of oral feeding, as the pH level and presence of amylase in saliva is more harmful to tissues than other liquids or food.
Early oral feeding, within 7 days of the operation, can reduce length of hospital stay.
A total laryngectomy causes the separation of the upper air respiratory tract, nose, mouth, and lower air respiratory tract, lungs, lower trachea.
Following laryngectomy breathing is no longer done through the nose, which causes a loss/decrease of the sense of smell, leading to a decrease in the sense of taste.
The Nasal Airflow Inducing Manoeuvre (NAIM), causes a negative pressure in the oral cavity, leading to an effective rehabilitation technique to improve the sense of smell.
Patients with a partial laryngectomy are more likely to have a higher quality of life than individuals with a total laryngectomy.
People having undergone total laryngectomy have been found to be more prone to depression and anxiety, and often experience a decrease in the quality of their social life and physical health.
Voice quality, swallowing and reflux are affected by partial and total laryngectomy, with the sense of smell and taste (hyposnia/anosmia and dysgeusia) also being affected in total laryngectomies.
Dysphagia affects quality of life following surgery with challenges in eating and social involvement, increased levels of distress.
People receiving voice rehabilitation report best voice quality and overall quality of life when using a voice prosthesis as compared to esophageal speech or electrolarynx.
Associated with impaired sense of smell and taste, increased incidence of tracheobronchial infections, stomal encrustation, loss of nasal respiration and loss of human-sounding voice.
