Affects 11-15% of the U.S. population 65 years of age and older.
Affects 3.4% of persons older in age 50 in the US.
Affects more than 14 million adults in the US.
Approximately 654 million people aged 40 years or older worldwide have knee osteoarthritis..
Knee osteoarthritis accounts for approximately 85% of the global disability burden of osteoarthritis.
Osteoarthritis of the knee is common, affecting 37% of persons 60 years of age or older
Estimated prevalence of KO in the elderly ranges from 6.9 to 15.4% worldwide.
its prevalence rises with increasing age.
Affects approximately 265 million people worldwide.
Obesity in young and mid-life increases risk.
Prevalence is rising due to an aging population and increased obesity.
In 2017 accounted for 8.3 million years lived with disability.
The process limits activity and impairs quality-of-life.
The risk of mobility disability associated with knee OA is greater than any other condition in people 65 years of age or older.
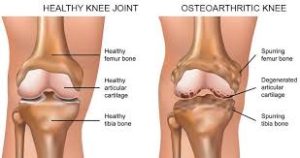
Characterized by articular cartilage loss, joint tissue remodeling, and inflammatory changes in the synovial membrane.
A chronic joint disorder manifesting as the structural and functional failure of synovial joints.
It is no longer considered a cartilage-centric/wear or tear disease because it affects the whole joint:local derangements of articular cartilage and subchondral bone, as well as alterations to the synovium, menisci, ligaments, and surrounding muscles and fat pads.
KO represents failed repair of joint damage resulting from stresses initiated by joint or periarticular tissues.
It’s pathogenesis is characterized by mechanical, inflammatory, and metabolic factors, leading to impaired balance between the repair and destruction of joint tissues.
Cartilage loss is fundamental to KO, but it is a disease of the whole joint.
Symptoms and signs of knee osteoarthritis: include pain, stiffness, reduced joint motion, muscle weakness, functional limitations, sensitivity, buckling, or giving way, bony enlargement and restricted range of motion.
Morning stiffness with KO lasts less than 30 minutes.
The knee pain in early stage OAis typically intermittent, predictable nociceptive in nature, and mostly present during weight-bearing.
Nociceptive pain may progressed to a more constant pain, reflecting eurobiological sensitization to stimuli.
Knee joint stiffness occurs after daytime inactivity.
Symptoms begin in men in their 40s or older and in women in perimenopause or older.
Potential long-term consequences of knee osteoarthritis include reduced physical activity, deconditioning, impaired sleep, fatigue, depression, functional decline, and disability.
KO long-term consequences include:
reduced physical activity,
deconditioning,
impaired sleep,
fatigue,
depression,
disability.
A discrepancy exists between the severity of symptoms and the severity of knee osteoarthritis on radiography.
This discrepancy may relate to pain sensitization, adaptation to chronic pain, or reduction in activity to avoid pain.
Pain from osteoarthritis of the knee fluctuates over time.
It episodic pain is predictable in early stages.
Knee pain becomes less predictable and more severe in late stages.
KO pain is often dull, involving the whole knee or more localized.
KO pain increases with use, and abates with rest.
Over time the pain may occur at rest and at night, interfering with sleep.
Factors associated with degree of knee pain in KO include: younger age, female sex, non-White race, lower educational level, obesity, burden of coexisting conditions, repetitive joint, usages, squatting, and kneeling, quadriceps muscle weakness. psychological factors, capacity to mobilize internal resources and actions to meet situational demands, tendency to magnify sensations and feel helpless, and pain sensitization.
Risk factors for functional impairment, and precursor of disability in KO: female sex, obesity, older age, falls, malalignment, previous in the injury, disease severity, and knee instability, whereas greater physical activity, strength, self-efficacy, and social support are associated with reduced risk.
Symptom severity and structural damage on imaging are commonly discordant.
Plain film radiography is not recommended for diagnosing knee OA.
The insensitivity of radiography may account for this discordance in early KO.
Radiography of the knees including weight-bearing posteroanterior view and patellofemoral, lateral or skyline view, may confirm osteoarthritis-related changes.
Radiographically changes include, osteophytes, subchondral sclerosis, cysts, bone attrition, and asymmetric joint-space narrowing.
Magnetic resonance imaging (MRI) may reveal disease manifestations in early disease. with normal radiographs.
The articular cartilage loss is a measure of structural disease progression, and is evaluated by MRI or indirectly by radiographs.
MRI provides a more accurate quantitative assessment of cartilage thickness than radiographs, and can predict the likelihood of future need for knee replacement with comparable or greater accuracy than x-rays.
About half of patients have radiographic evidence of degenerative disease of the knee and many have changes not visible on radiography.
Findings may be worse in the medial or lateral tibiofemoral or patellofemoral compartments, or may involve a combination of the tibiofemoral and patellofemoral compartments.
Despite its almost universal use, MRI is indicated only in rare circumstances: persistent mechanical symptoms and objective locking, which would possibly indicate a displaced meniscal tear.
Symptom severity and structural damage discordance may also relate to pain sensitization of the nociceptive processing in the peripheral or central nervous system, and adaptation to chronic pain, or reduction in activity to avoid pain.
Pathologically due to excessive mechanical stress in the context of systemic susceptibility.
Pathological changes occur in subchondral bone, and periarticular bone: ranging from trabecular thickening to pathological disruption.
Periarticular bone contributes to loading force dispersion across the joint, and changes in it can further predispose the knee joint to osteoarthritis.
The synovial fluid from a patient with osteoarthritis of the knee has less viscosity and less elasticity than from patients with a normal knee.
In osteoarthritis the viscoelasticity of synovial fluid is reduced, in part due to decreases in the molecular weight and concentration of endogenous hyaluronic acid.
Weight is top risk factor for knee osteoarthritis and pain.
Other factors include female gender, previous knee injury, age, and presence of hand osteoarthritis..
One-fourth of cases of onset of knee pain could be attributable to being either overweight or obese,
Prevalence increases with age and is more common in women.
Major risk factors include obesity, prior knee injury, previous knee surgery and occupation bending and lifting.
Factors that have been associated with an increased risk of KO include: older age, female sex, overweight or obesity, knee injury, occupational factors associated with knee bending, heavy lifting, and squatting, and varus or valgus alignment.
Risk of KO is not increased with recreational physical activity.
Osteoarthritis of the knee prevalence is increasing.
Medial osteoarthritis is one of the most common subtype of osteoarthritis of the knee.
May be part of a generalized process of osteoarthritis.
A medical history and physical examination are usually sufficient to establish the diagnosis of osteoarthritis.
One or both knees may be affected: with or without more generalized osteoarthritis.
Symptoms of KO begin gradually.
Clinical findings of KO include: crepitus, bony enlargement, reduced knee flexion, flexion contracture, and tenderness.
Erythema, warmth, and swelling are mild, if present, but if significant
suggests another process.
Fixed or dynamic malalignment and instability on standing.
Natural history includes improvement, stability and worsening.
Acetaminophen, nonsteroidal anti-inflammatory drugs and analgesics are the same most commonly used treatments, but have limited effectiveness and are associated with adverse effects.
Injected intra-articular anesthetic reduces pain in 6 of 10 persons suggesting that in some patients, pain originates from extra-articular sources.
Implicated as a risk factor for falls in the elderly.
A 5.1 kg loss in body mass over a 10-year period decreases the odds of developing knee osteoarthritis by over 50%.
Leading cause of impaired mobility in elderly patients.
Many patients have impaired function preventing them from engaging in their usual activities.
Affects all structures within a joint.
Hyaline articular cartilage is lost, bone remodeling occurs, capsular stretching occurs and periarticular muscle weakness manifests.
Pain control remains poor in more than half of patients.
The use of cholecalciferol (vitamin D) dioes not improve Fixed or dynamic malalignment and instability on standing.knee pain or cartilage volume loss in patients with severe knee osteoarthritis .
Vitamin D supplements has no impact on the pain of knee osteoarthritis (OA).
A meta-analysis of using lateral wedge treatments and shoes and insoles designed to reduce medial compartment loading to reduce knee pain in medial knee osteoarthritis indicated no efficaciousness (Parkes MJ et al).
Arthroscopic surgery for degenerative meniscal tears in patients with mild knee osteoarthritis has no benefit for function or pain as analyzed by a meta-analysis.
A partial arthroscopic meniscectomy has been frequently performed in patients who have knee osteoarthritis with meniscal damage, but a meta-analysis of nine randomized trials comparing this procedure with nonsurgical treatments, including physical therapy, showed small benefits of uncertain clinical significance in the 6 months after surgery that dissipates by 1-2 years: no significant improvement in knee function results.
Arthroscopic surgery for knee osteoarthritis was shown in a sham controlled randomized trial that this procedure conferred no benefit over placebo.
Many patients with knee osteoarthritis (OA) also have degenerative meniscal tears, and while previous randomized trials found no benefit for arthroscopic surgery with severe arthritis, the role of the surgery in the context of milder OA is less clear.
A systematic review of the literature, identifying seven randomized trials with all patients having documented degenerative meniscal tears: found no improvement with surgery.
Guidelines strongly recommended against arthroscopic partial meniscectomy in nearly all patients with knee osteoarthritis, with the possible exception of those who had objective knee locking.
In patients with advanced osteoarthritis whose pain is not controlled with other interventions, knee replacement should be considered.
No drugs are currently approved as osteoarthritis disease modifying agents.
No medical treatments influence the course of the disease.
Guidelines for the treatment of knee osteoarthritis emphasizes education, exercise, weight loss, if appropriate, rather than the use of drugs or surgery.
Exercise and physical therapy with strengthening muscles around joints is the most important part of treatment of osteoarthritis.
In a randomized clinical trial of 823 patients with knee osteoarthritis and overweight or obesity treated with diet and exercise, versus attention control was met with a statistical significant difference: It however the small difference in the pain was of uncertain clinical importance (Messier SP).
Physical therapy has similarly effectiveness in the short term and better in the long term than a glucocorticoid injection.
Treatments for knee osteoarthritis (KO): education, physical activity including exercise and weight management.
Current approaches of treatment are focused on relieving symptoms, as no treatment has been identified for disease modification
Topical nonsteroidal antiinflammatory drugs (NSAIDs) are a first-line treatment for knee osteoarthritis.
Topical NSAIDs have benefits similar to that with oral NSAIDs but with fewer adverse effects.
If topical treatment is inadequate or not feasible, treatment often involves either an oral NSAID plus a proton-pump inhibitor or a cyclooxygenase-2 (COX-2) inhibitor.
Patients with osteoarthritis of the knee who undergo physical therapy have less pain and functional disability at one year than patients who receive an intra-articular glucocorticoid injection (Deyle GD).
Objective measured daily activity is not associated with a one-year symptom improvement among community dwelling adults with knee osteoarthritis (Liu,SH).
In the above study in patients with advanced knee arthritis greater daily minutes and physical activity was associated with worsening symptoms.
Oral agents such as acetaminophen, and nonsteroidal anti-inflammatory drugs are utilized to control pain.
The use of glucosamine or chondroitin sulfate or products containing a combination of these compounds did not lead to greater reductions in joint pain than placebo.
Duloxetine, a serotonin and norepinephrine reuptake inhibitor that has antidepressant, central pain inhibitory, and anxiolytic activities, is efficacious in patients with knee osteoarthritis.
Duloxetine may be particularly useful in patients who have widespread pain or depression.
Topical gel and solution formulations of non-steroid all anti-inflammatory drugs diclofenac (Voltaren) are modestly effective in reducing pain with a low risk of systemic adverse effects.
For patients with in adequate response or contraindications to systemic anti-inflammatory or analgesic drugs intra-articular corticosteroid and hyaluronic acid injections are used.
Intraarticular glucocorticoid injections are commonly used, because they are easy to administer, involve fewer visits, and patient adherence is not an issue.
Intraarticular glucocorticoid injection benefits are short-lived, and associated with adverse effects on the joint with a small increase in loss of quarterly volume of uncertain clinical relevance.
Glucocorticoid injections are efficacious for short-term pain relief.
Regular injections with triamcinolone, administered intraarticularly every 3 months, resulted in greater loss of cartilage volume than saline injections.
There is insufficient evidence to support a meaningful effect of intraarticular hyaluronic acid.
A meta-analysis using intraarticular hyaluronic acid showed modest effect sizes and a risk of serious adverse events, such as injection-site reaction and joint swelling.
Biomechanical treatments for knee osteoarthritis are intended to reduce pain, improve physical function, and potentially slow disease progression, but evidence of their effectiveness has been inconclusive.
The use of biomechanical footwear compared with controlled footwear resulted in an improvement in the pain at 24 weeks and was statistically significant, but the difference was of uncertain clinical importance (Reichenbach S).
In a randomized controlled study of physical therapy versus intra-articular glucocorticoid injections results indicated that the patients with physical therapy had less pain and functional disability at one year than patients in the glucocorticoid injection group.
Clinical findings do not support the use of bisphosphonates to slow cartilage volume loss in patients with knee osteoarthritis.
High intensity strength training compared with low intensity strength training does not significantly reduce knee pain impatience with knee osteoarthritis.
Tramadol may be considered in very limited contexts in which NSAIDs are contraindicated or ineffective and the pain is severe.
No role for other opioids in the management of osteoarthritis.
Among patients with symptomatic mild to moderate radiographic knee osteoarthritis, intra-articular injection of plasma rich platelets compared with injection of saline placebo, did not does not significantly result in a difference in symptoms or join structure at 12 months: not supporting the use of plasma rich platelets for the management of osteoarthritis.
Indications for a surgical intervention is typically end stage osteoarthritis defined as no or minimal joint space with inability to cope with pain after conservative options have not effectively relieved symptoms.

One reply on “Knee osteoarthritis”
[…] See ((Knee osteoarthritis)) […]