
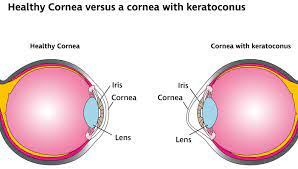
 A progressive, non-inflammatory process, with bilateral ectatic corneal disease with paraxial stromal thinning and weakening leading to corneal surface distortion.
A progressive, non-inflammatory process, with bilateral ectatic corneal disease with paraxial stromal thinning and weakening leading to corneal surface distortion.
Keratoconus is a bilateral, progressive, asymmetric, non-inflammatory thinning condition of the cornea.
A non-inflammatory disorder, characterized by corneal thinning and bulging outside in the cone shape.
Starts typically between the ages of ten and thirty years of age.
The incidence is greater than 1in 2000 patients per year.
Prevalence higher in zones with higher ultraviolet exposure.
Manifests with a high degree of irregular astigmatism, causing visual blur and distortion.
Vision impairment often not correctible with eyeglasses or ordinary contact lenses, and most patients will require special rigid contact lenses.
As many as 20% of patients eventually require a corneal transplant.
Diagnosis is made usually in late stage, with significant vision loss.
Irregular astigmatism results as does myopic vision from corneal scarring.
Involvement of the axial and infernasal cornea is typical.
All layers of the cornea affected with basement membrane fragmentation and scarring.
Bowman membrane, the anterior limiting lamina has breaks.
Fleisher ring due to iron deposition in the basal layer epithelial cells occurs.
Breaks and fold in Descemet membrane may result in striae and rarely acute hydrops.
Associated with altered antioxidant enzyme activity, accumulation of oxygen/nitrogen cytotoxic reactive species, activation of capsase patheays, and DNA mitochondrial damage.
Oxidative stress elements found in corneal cells and can induce degradative enzymes and inhibit degradation of tissue metal-low proteinases.i
Mild keratoconus is associated with irregular astigmatism.
Mild keratoconus may be confirmed with computer assisted video keratography, which may reveal corneal inferior steepening, sensual, corneal a stigmatism or even bilateral temporal steepening.
Moderate keratoconus may have enhanced appearance of the corneal nerves, fine stress lines in the deep stromal cornea in about 40% of cases, and approximately 50% develop iron deposition in the basal epithelial cells, the Fleisher ring, an approximate 20% develop corneal scarring.
Not associated with increased mortality.
Seen uncommonly in elderly.
Acute keratoconus, corneal hydrops, is rare and occurs when the Descemet layer develops breaks through which aqueous fluid can enter the central stroma causing edema and corneal scarring.
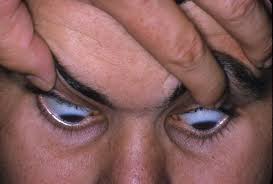
In advanced cases, an eyelid deflection can be noted – Munson’s sign.
In acute keratoconus acute loss of vision may occur.
Deletion of SOD1 (superoxide dismutatse) gene associated wit the process.
50-200 cases per 100,000 population.
Mostly an isolated finding, but may be associated with systemic process.
Associated ocular lesions include vernal conjunctivitis, retinitis pigmentosa, and Leber congenital amaurosis.
Associations include connective tissue diseases including Ehlers-Danlos syndrome, Marfan’s syndrome.
May be associated with Down syndrome, mitral valve prolapse and atopic dermatitis.
Risk factors include atopic immune disease, ocular allergies, use of rigid contact lenses and vigorous eye rubbing.
14% of cases have a genetic transmission.
Most cases are spontaneous.
Corneal collagen crosslinking is an effective treatment for early to moderate keratoconus.
Corneal collagen crosslinking can stop the progression of the disease, but cannot predictably reverse vision loss once it has already occurred.
The condition is treated by corneal collagen cross-linking, which increases corneal stiffness.
Cross-linking is achieved by applying a topical riboflavin solution to the cornea, which is then exposed to ultraviolet A light.
