 Keratinocytes are the primary type of cell found in the outermost layer of the skin, the epidermis.
Keratinocytes are the primary type of cell found in the outermost layer of the skin, the epidermis.
Their primary function is the formation of a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses.
Keratinocytes constitute 90% of epidermal skin cells.
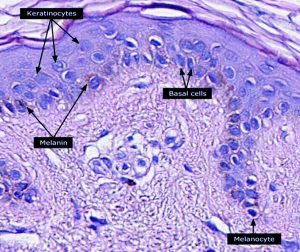
Basal cells in the basal layer of the skin are sometimes referred to as basal keratinocytes.
Keratinocytes form a barrier against environmental damage: heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses.
In addition to keratinocytes, structural proteins, enzymes, lipids, and antimicrobial peptides contribute to maintain barrier function of the skin.
Keratinocytes differentiate from epidermal stem cells in the lower part of the epidermis and migrate towards the surface.
They become corneocytes and eventually are shed off, every 40 to 56 days in humans.
Invading pathogens to the upper layers of the epidermis can cause keratinocytes to produce proinflammatory mediators.
These chemokines such as CXCL10 and CCL2 attract monocytes, natural killer cells, T-lymphocytes, and dendritic cells to the site of pathogen invasion.
The barrier function of the skin is maintained by a number of structural proteins, filaggrin, and keratin, protease enzymes, lipids, and antimicrobial peptides, and defensins.
Keratinization or cornification, in which the keratinocytes produce more and more keratin is part of the physical barrier formation
The fully cornified keratinocytes that form the outermost layer are constantly shed off and replaced by new cells.
The epidermal stem cells reside in the lower part of the epidermis, known as the stratum basale.
The epidermal cells are attached to the basement membrane through hemidesmosomes.
Epidermal stem cells divide, yielding either more stem cells or transit amplifying cells.
Stem cells and their differentiated progeny are organized into columns named epidermal proliferation units.
Keratinocytes subsequently withdraw from the cell cycle, express epidermal differentiation markers, and move suprabasally as they become part of the stratum spinosum, stratum granulosum, and eventually corneocytes in the stratum corneum.
Corneocytes are keratinocytes that have completed their differentiation program and have lost their nucleus and cytoplasmic organelles, and eventually be shed off through desquamation as new ones come in.
Keratinocytes express specific keratins, such as keratin 1, keratin 5, keratin 10, and keratin 14.
Keratinocytes also expressmarkers such as involucrin, loricrin, transglutaminase, filaggrin, and caspase 14.
It is estimated that keratinocytes turn over from stem cells to desquamation every 40–56 days.
A calcium gradient exists on keratinocytes, with the lowest concentration in the stratum basale and increasing concentrations until the outer stratum granulosum, where it reaches its maximum.
Vitamin D3, cholecalciferol, regulates keratinocyte proliferation and differentiation.
Vitamin D3 modulates calcium concentrations and regulates the expression of genes involved in keratinocyte differentiation.
Keratinocytes are the only cells in the body with the entire vitamin D metabolic pathway from vitamin D production to catabolism and vitamin D receptor expression.
Keratinocyte differentiation inhibits keratinocyte proliferation.
Factors that promote keratinocyte proliferation should be considered as preventing differentiation.
Transcription factor p63, prevents epidermal stem cells from differentiating into keratinocytes.
Mutations in the p63 DNA-binding domain are associated with ectrodactyly, ectodermal dysplasia, and cleft lip/palate (EEC) syndrome.
The transcriptome of p63 mutant keratinocytes deviated from the normal epidermal cell identity.
In the epidermis keratinocytes are associated with other cell types such as melanocytes and Langerhans cells.
Keratinocytes form tight junctions with the nerves of the skin and hold the Langerhans cells and intra-dermal lymphocytes in position within the epidermis.
Keratinocytes are producers of anti-inflammatory mediators such as IL-10 and TGF-β, and can stimulate cutaneous inflammation and Langerhans cell activation via TNFα and IL-1β secretion.
They protect the body from ultraviolet radiation (UVR) by taking up melanosomes, vesicles containing the endogenous photoprotectant melanin, from epidermal melanocytes.
Each melanocyte in the epidermis has several dendrites that connect it with many keratinocytes.
Melanin is then stored within keratinocytes and melanocytes protect the DNA from UVR-induced damage.
Skin wounds to the skin will be repaired in part by the migration of keratinocytes to fill in the gap created by the wound.
The keratinocytes to participate in that repair come from the hair follicle and only survive transiently.
They will be replaced by keratinocytes originating from the epidermis.
Functional keratinocytes are required for tympanic perforation healing.
A sunburn cell is a keratinocyte with a pyknotic nucleus and eosinophilic cytoplasm that appears after exposure to UVC or UVB radiation or UVA in the presence of psoralens.
A sunburned cell shows premature and abnormal keratinization, and is described as an example of apoptosis.
With age, stem/progenitor cells fail to self-renew or differentiate.
DNA damage caused by exposure of stem/progenitor cells to reactive oxygen species (ROS) may play a key role in epidermal stem cell aging.
A Civatte body is a damaged basal keratinocyte that has undergone apoptosis, and consist largely of keratin intermediate filaments, and are almost invariably covered with immunoglobulins, mainly IgM.
Civatte bodies are characteristically found in skin lesions of various dermatoses, particularly lichen planus and discoid lupus erythematosus.
Civatte bodies may be found in graft-versus-host disease, adverse drug reactions, inflammatory keratosis, erythema multiforme, bullous pemphigoid, eczema, lichen planopilaris, febrile neutrophilic dermatosis, toxic epidermal necrolysis, herpes simplex and varicella zoster lesions, dermatitis herpetiformis, porphyria cutanea tarda, sarcoidosis, subcorneal pustular dermatosis, transient acantholytic dermatosis and epidermolytic hyperkeratosis.
