Leiomyoma the most frequent indication for abdominal hysterectomy.
Most common non-obstetric major surgery among women in the United States.
There is a declining rate of hysterectomy, hysterectomy with and without concomitant oophorectomy.
Salpingectomy remains the second most common surgical procedure for women in the United States.
The cumulative incidence of hysterectomy approaches 50% in the United States.
Less than 10% of hysterectomies are performed for any type of cancer or precancer.
Oophorectomy and salpingectomy are often performed without pathologic diagnoses but, instead, with the intent to prevent ovarian cancer.
One in nine women in the United States will undergo this procedure during her lifetime.
Approximately 600,000 per year in the U.S.
Estimated that by age 64 years 40% of women will have had a hysterectomy.
20% for menorrhagia.
90% of cases are from benign gynecologic conditions.
Increases the long-term risk of incontinence.
Bleeding complications 1-3% of cases.
Six-week recovery period.
15-38% risk of a postoperative febrile illness.
Standard of care for endometrial cancer and traditionally performed through a laparotomy, but is associated with substantial perioperative morbidity.
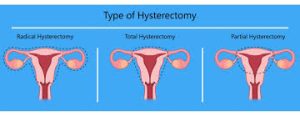
Traditionally performed abdominally via laparotomy, vaginally, or laparoscopically, and now robotically assisted hysterectomy is an alternative minimally invasive procedure.
Intraoperative hemorrhage in 0.2-3.7% of cases.
Postoperative hemorrhage more common after vaginal than abdominal hysterectomy, 1.9% vs. 1.6%.
Transfusion requirement with hysterectomy 1-5%.
Laparoscopic hysterectomy transfusion requirement 2.1%.
Laparoscopic hysterectomy early and late postoperative hemorrhage rate reported as 0.2% and 0.5%, respectively.
Compared with opened hysterectomy, laparoscopic procedure as less morbidity, short hospital days, and is the preferred treatment for many.
Robotic as an alternative minimal invasive surgical procedure.
Approximately half of all postoperative fevers after vaginal and abdominal hysterectomy have no identifiable source.
Approximately 32% of patients undergoing abdominal hysterectomy and approximately 16.8% undergoing vaginal hysterectomy have postoperative fever.
After abortion is most commonly performed for hemorrhage.
Hysterectomy for benign reasons associated with renal cancer (Altman D et al).
Increases risk of renal cancer after hysterectomy by 50%.
Women undergoing hysterectomy at an earlier age have a higher risk of developing renal cancer.
Patients followed for an average of 20 years after hysterectomy, even with conservation of both ovaries, the procedure is associated with substantial medical complications including: risk of heart disease, mental health conditions.
It is suggested that uteropelvic junction obstruction and persistent subclinical hydronephrosis after hysterectomy may predispose to renal proliferation and cancer transition (Gago-Dominguez M et al).
Elective bilateral salpingo-oophorectomy is generally offered to women 40 years of age or older at the time of the procedure to prevent the development of ovarian cancer.
Bilateral salpingo-oophorectomy is performed in 40% of benign hysterectomies among women age 40-44 years, 60% among women aged 45-50 years, and 70% among women age 50-55 years ( Whiteman MK et al, Jacoby VL et al).
Most patients undergoing hysterectomy are premenopausal so that BSO results in abrupt decline in ovarian hormone levels that may result in menopausal symptoms.
Since the Women’s Health Initiative (WHI) the routine use of postmenopausal hormone therapy has made the elective performance of BSO more controversial.
Among more than 25,000 women without a family history of ovarian cancer who had a hysterectomy, those keeping their ovaries were later diagnosed with ovarian cancer at a rate of 0.33%, compared with 0.02% in the women who also had elective bilateral salpingo-oophorectomy ( Jacoby VL et al).
In the above study no evidence of increased morbidity or mortality among the women choosing simultaneous BSO and hysterectomy, and cardiovascular events, hip fracture, and breast cancer were no more common in women undergoing BSO than in those choosing ovarian conservation.
Hysterectomy is associated with the small, but significantly increased risk of cardiovascular disease, independent of removal of the ovaries, with an increased mortality risk among those who undergo hysterectomy before age 40.
Current guidelines from the American Congress of Obstetricians and Gynecologists recommends BSO for women known to be at risk for ovarian cancer but ovarian preservation in those without such risk.
The above findings are from the Women’s Health Initiative Observational Study, which enrolled 25,448 postmenopausal women who had previously had hysterectomies and no family history of ovarian cancer with slightly more than half (56%) had also undergone BSO along with the hysterectomy.
Robotic surgery allows the performance of this procedure from a remote console.
Robotic surgery increases range of motion with instrumentation, provides three-dimensional stereoscopic visualization, and improved ergonomics for the surgeon.
Robotic hysterectomy is not associated with improved effectiveness or safety.
The perioperative morbidity is similar for robotic assisted and laparoscopic hysterectomy, while robotic assisted hysterectomy is substantially more expensive than any other type of hysterectomy.
