 Characterized by fibrosis and thickening of the duramater with resulting neurological dysfunction.
Characterized by fibrosis and thickening of the duramater with resulting neurological dysfunction.
Labeled as idiopathic hypertrophic pachymeningitis in the absence of any definite inciting factor
May be related to inflammatory and infectious conditions.
Common clinical features include headaches, multiple cranial nerve palsies and cerebellar dysfunction ocurring alone or in combination.
Described as primary or idiopathic hypertrophic pachymeningitis where no identifiable cause is found.
Described as secondary where identifiable causes exist, although their definite relationship to the development of this condition may be debatable.
A diagnosis of exclusion.
Pathogenesis is unknown, although autoimmunity may be responsible, or occur as a result of infectious or infiltrative pathology.
A process of encasement of brain tissue by thickened and fibrous meninges with resultant clinical symptomatology.
While the disease may be focal or multicentric in presentation, the main symptoms are headache, cranial neuropathies and cerebellar dysfunction.
Spinal pachymeningitis manifesting as a radiculopathy, myelopathy or a combination of the two, can occur alone or as a craniospinal form.
Headaches can be focal or diffuse.
Headaches may be the only symptom for years before other symptoms manifest.
Cranial neuropathies are present in all the cases.
Lower cranial nerve involvement, especially VIII and X, are most common.
Almost any cranial nerve except I can be involved.
There are 2 patterns of cranial nerve involvement based on the site of dural inflammation.
Anterior involvement presents with paresis of II-VI cranial nerves.
Posteriorly, cranial nerves V to XII may be involved, with involvement of VIII nerve being the most common.
It is suspected that the dense fibrous encasement and ischemic damage by hypertrophic tissue explains the cranial nerve deficits.
Optic neuropathy is uncommon as is cerebellar dysfunction.
Uncommon clinical presentations include encephalitis, pan hypo-pituitarism, diabetes inspidus, sinus thrombosis and hydrocephalus.
Spinal pachymeningitis commonly involves the cervico-dorsal dura and presents with features of radiculopathy and/or myelopathy.
Diagnosis requires excluding all possible causes including: infectious, noninfectious and malignant etiologies.
CSF studies are inconclusive and usually report lymphocytic pleocytosis with variable increase in cell counts, moderately elevated protein levels, but may be normal.
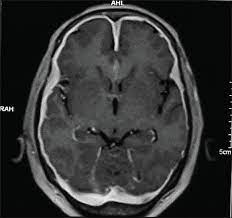
Imaging shows a pachymeningeal changes.
Thickening of dura mater is observed.
Non-enhanced CT scans show thickened, hyperdense dura, typically along the tentorium, tentorial ridge, falx and prepontine brain stem.
Enhanced brain CT scans show marked enhancement on contrast administration.
The thickened dura on MR images usually shows a uniform dense enhancement of the thickened membranes.
A dural biopsy differentiates idiopathic from secondary forms of pachymeningitis.
Histology features include thickening, fibrosis and presence of inflammatory cells including plasma cells and lymphocytes.
The presence of granulomas or vasculitis help in establishing a specific diagnosis.
Diagnosis of idiopathic form is one of exclusion.
Tuberculosis, syphilitic pachymeningitis, and neurosarcoidosis should be considered in the differential diagnosis of any dural based lesion.
Neurosarcoidosis causes non-caseating granulomas with predilection for bilateral facial nerve involvement.
Associated mononeuritis multiplex has been reported in up to 28% of the patients.
The progression of this disease is more rapid and potentially fatal as compared to hypertrophic pachymeningitis of uncertain etiology.
Evidence of necrotising vasculitis on biopsy, and positive ANCA can aid in establishing the diagnosis.
Intracranial hypotension is an important cause of meningeal enhancement, with postural headaches, occasionally abducens palsy and low CSF pressures occurring spontaneously or following craniotomy, shunt placement, lumbar puncture, head trauma or dural tears.
The intense dural enhancement that occurs possibly related to compensatory increase in venous blood secondary to reduced CSF volume and pressure.
Hypertrophic pachymeningitis might also be related to a group of disorders with fibrosclerotic tendency such as sclerosing cholangitis, or episcleritis.
Steroid therapy has been considered the mainstay of therapy in this disease.
However, the disease progression might continue despite institution of steroids and many patients may eventually become steroid dependent,.
Immunomodulating agents like azathioprine and cyclophosphamide have been tried, although the efficacy has not been proven.
Combined therapy with steroids and azathioprine has been used with improvement.
Decompressive surgery has been used for spinal and orbital lesions.
An important cause of recurrent cranial neuropathies and headaches, but infectious, inflammatory, non-infectious and malignant conditions can produce a similar picture.
Aim of the therapy is to prevent permanent damage to neural tissue.
